Adequate vascular access is essential for proper dialysis. Native arteriovenous (AV) fistulas are the first choice for hemodialysis.1,2
Establishing hemodialysis access and monitoring and management of vascular access complications is a challenge that involves several specialties and healthcare settings, including nephrologists, radiologists, vascular surgeons and nephrology nurses.3,4
The need for coordination between specialists to optimize results has been emphasized.5–7 Clinical guidelines recommend the creation of multidisciplinary teams in each center dedicated to vascular access.1
In 2015 we started to build a multidisciplinary unit dedicated to the creation and treatment of vascular accesses in our health area, which includes two university hospitals and three hemodialysis centers. We drafted and agreed common protocols for action and began implementing them. In 2017, we completed the implementation process and began the evaluation and updating phase.
The multidisciplinary team is composed of a nephrologist from each of the hemodialysis units, a vascular surgeon, an interventional radiologist from each of the hospitals and a nursing representative from each unit. The team was responsible for drafting the protocols and clinical pathways, as well as for data collection and analysis of annual results.
Every week we have 2 monographic clinics for consultations on vascular accesses attended by a vascular surgeon, a nephrologist and a nurse from the multidisciplinary team. They assess new patients who are candidates for vascular access and review any accesses with problems. Joint nephrology, vascular surgery and radiology sessions are scheduled depending on the cases to be assessed. On a weekly basis, there is an outpatient major surgery operating room reserved for vascular accesses and those interventions requiring hospitalization are programmed in the available slots in the general operating rooms. Scheduling priorities are also managed by the team in accordance with the parameters established in the clinical guidelines. Emergencies are attended by the regular nephrology and vascular surgery on-call team and subsequently referred to the access consultation for review.
To evaluate the results, we performed a retrospective cross-sectional study comparing two groups of patients: those undergoing AV fistula creation or treatment from January 2015 to December 2017 (historical group A, n = 294) and from January 2018 to December 2019 (group B, after device implantation, n = 323). The type of procedure performed, time on waiting list, maturation rate at 60 days, AV fistula survival, frequency of catheters in both incident and prevalent patients, as well as results on 14 quality indicators in both groups were analyzed.
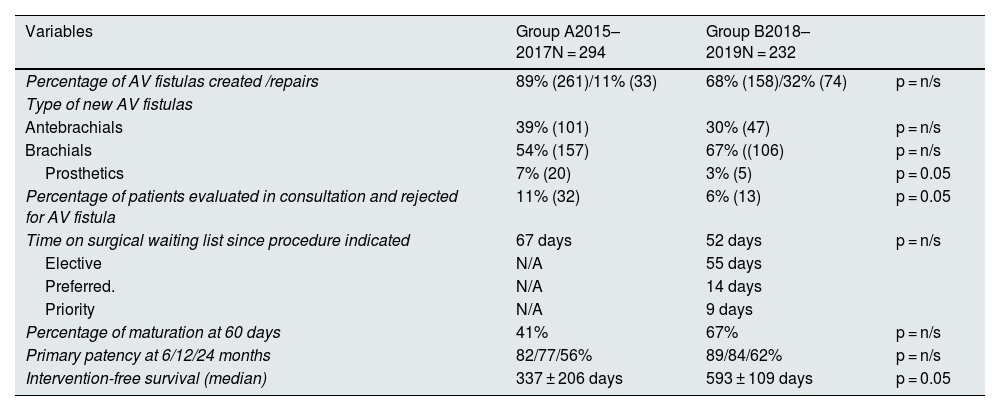
The results of the analysis are in Tables 1 and 2.
Results of variables analyzed.
| Variables | Group A2015–2017N = 294 | Group B2018–2019N = 232 | |
|---|---|---|---|
| Percentage of AV fistulas created /repairs | 89% (261)/11% (33) | 68% (158)/32% (74) | p = n/s |
| Type of new AV fistulas | |||
| Antebrachials | 39% (101) | 30% (47) | p = n/s |
| Brachials | 54% (157) | 67% ((106) | p = n/s |
| Prosthetics | 7% (20) | 3% (5) | p = 0.05 |
| Percentage of patients evaluated in consultation and rejected for AV fistula | 11% (32) | 6% (13) | p = 0.05 |
| Time on surgical waiting list since procedure indicated | 67 days | 52 days | p = n/s |
| Elective | N/A | 55 days | |
| Preferred. | N/A | 14 days | |
| Priority | N/A | 9 days | |
| Percentage of maturation at 60 days | 41% | 67% | p = n/s |
| Primary patency at 6/12/24 months | 82/77/56% | 89/84/62% | p = n/s |
| Intervention-free survival (median) | 337 ± 206 days | 593 ± 109 days | p = 0.05 |
AV fistula: arteriovenous fistula.
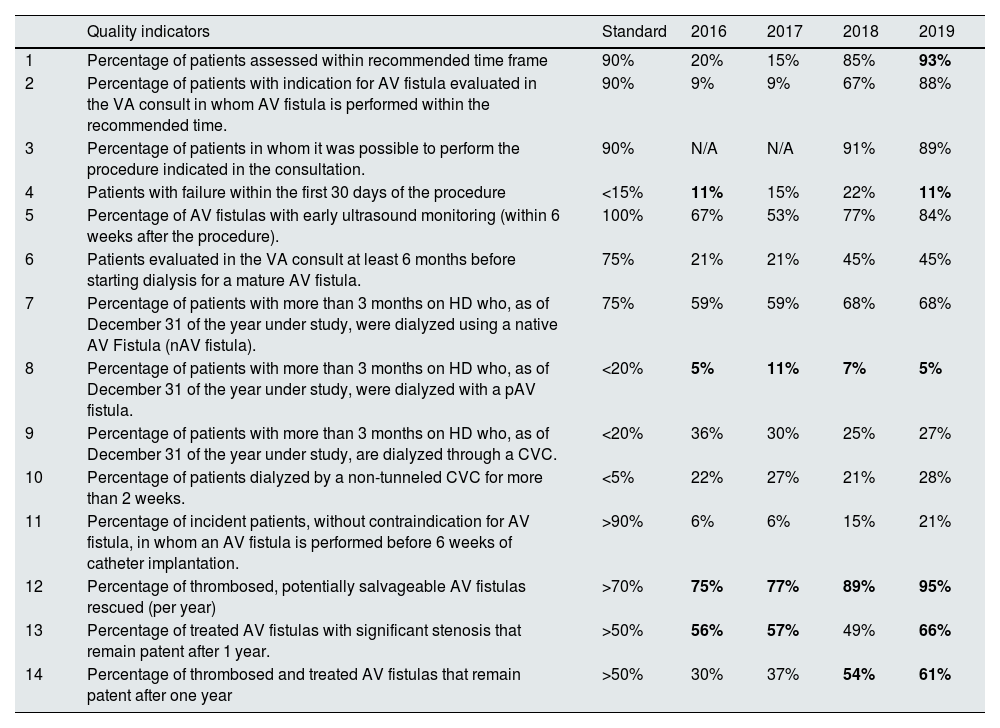
Results of quality indicators analyzed.
| Quality indicators | Standard | 2016 | 2017 | 2018 | 2019 | |
|---|---|---|---|---|---|---|
| 1 | Percentage of patients assessed within recommended time frame | 90% | 20% | 15% | 85% | 93% |
| 2 | Percentage of patients with indication for AV fistula evaluated in the VA consult in whom AV fistula is performed within the recommended time. | 90% | 9% | 9% | 67% | 88% |
| 3 | Percentage of patients in whom it was possible to perform the procedure indicated in the consultation. | 90% | N/A | N/A | 91% | 89% |
| 4 | Patients with failure within the first 30 days of the procedure | <15% | 11% | 15% | 22% | 11% |
| 5 | Percentage of AV fistulas with early ultrasound monitoring (within 6 weeks after the procedure). | 100% | 67% | 53% | 77% | 84% |
| 6 | Patients evaluated in the VA consult at least 6 months before starting dialysis for a mature AV fistula. | 75% | 21% | 21% | 45% | 45% |
| 7 | Percentage of patients with more than 3 months on HD who, as of December 31 of the year under study, were dialyzed using a native AV Fistula (nAV fistula). | 75% | 59% | 59% | 68% | 68% |
| 8 | Percentage of patients with more than 3 months on HD who, as of December 31 of the year under study, were dialyzed with a pAV fistula. | <20% | 5% | 11% | 7% | 5% |
| 9 | Percentage of patients with more than 3 months on HD who, as of December 31 of the year under study, are dialyzed through a CVC. | <20% | 36% | 30% | 25% | 27% |
| 10 | Percentage of patients dialyzed by a non-tunneled CVC for more than 2 weeks. | <5% | 22% | 27% | 21% | 28% |
| 11 | Percentage of incident patients, without contraindication for AV fistula, in whom an AV fistula is performed before 6 weeks of catheter implantation. | >90% | 6% | 6% | 15% | 21% |
| 12 | Percentage of thrombosed, potentially salvageable AV fistulas rescued (per year) | >70% | 75% | 77% | 89% | 95% |
| 13 | Percentage of treated AV fistulas with significant stenosis that remain patent after 1 year. | >50% | 56% | 57% | 49% | 66% |
| 14 | Percentage of thrombosed and treated AV fistulas that remain patent after one year | >50% | 30% | 37% | 54% | 61% |
VA, vascular access; CVC, central venous catheter; AV, arteriovenous; nAV, native arteriovenous; pAV, prosthetic arteriovenous; HD, hemodialysis.
Description: Annual evolution of quality indicators between 2016 and 2018. Results that met the marked standard are marked in bold.
In conclusion, the development of a multidisciplinary team following a protocol has allowed a decrease in the waiting time between evaluation in consultations and AV fistula creation. There has been an increase in the survival rate of group B AV fistulas. In turn, there has been a significant improvement in compliance with quality indicators.
Having a fixed consultation clinic and an operating room per week has allowed us to manage both agendas and to schedule patients according to their needs. However, the improvement in the indicators for preferential or priority patients has not had an impact on the overall number of waiting days; for each preferential or priority patient whose surgery was brought forward, one elective patient was delayed. In order to observe a more marked overall decrease in wait time, it would be necessary to increase the number of total annual operating room slots according to the existing demand.
Although we have improved the rate of patients evaluated in consultations clinic who initiated HD due to AV fistula, the rate of catheter use in prevalent patients has hardly changed, especially in tertiary hospital units. This may be due to different variables, authors such as Liebman and Chang8 and Gomis Couto et al.9 have suggested that the initiation of dialysis by CVC is more frequently due to a flare-up of previously stable renal disease due to intercurrent disease than to a late referral to nephrology consultation, these patients are mainly found in the units of second and third level centers. In peripheral centers, the biggest problem has been the refusal of patients with CVC to undergo AV fistula. This variable has already been analyzed in the literature, the fact of starting HD with a CVC negatively predisposes patients to have an AV fistula and this refusal increases the longer they have had the CVC,10 so it is important not to delay the creation of an AV fistula in patients attended in the centers.