The 2019 coronavirus (COVID-19) is a viral infection caused by a new coronavirus that is affecting the entire world. There have been studies of patients on in-center hemodialysis (HD), but home dialysis population data are scarce. Our objective is to study the incidence and course of COVID-19 in a home dialysis unit (HDU) at the height of the pandemic.
Methodsan observational, retrospective study enrolling all patients diagnosed with COVID-19 from the HDU of Hospital Universitario La Paz [La Paz University Hospital] (Madrid, Spain) between March 10 and May 15, 2020. We collected clinical data from the HDU (57 patients on peritoneal dialysis [PD] and 22 patients on home hemodialysis [HHD]) and compared the clinical characteristics and course of patients with and without COVID-19 infection.
Resultstwelve patients were diagnosed with COVID-19 (9 PD; 3 HHD). There were no statistically significant differences in terms of clinical characteristics between patients with COVID-19 and the rest of the unit. The mean age was 62 ± 18.5 years; most were men (75%). All patients but one required hospitalization. Ten patients (83%) were discharged following a mean of 16.4 ± 9.7 days of hospitalization. Two patients were diagnosed while hospitalised for other conditions, and these were the only patients who died. Those who died were older than those who survived.
ConclusionThe incidence of COVID-19 in our HDU in Madrid at the height of the pandemic was high, especially in patients on PD. No potential benefit for preventing the infection in patients on home dialysis was observed. Advanced age and nosocomial transmission were the main factors linked to a worse prognosis.
La enfermedad por coronavirus 2019 (COVID-19) es una infección viral causada por un nuevo coronavirus que está afectando a todo el mundo. Hay estudios previos de pacientes en hemodiálisis en centro (HD), pero hay pocos datos sobre población en diálisis domiciliaria. Nuestro objetivo es estudiar la incidencia y evolución de COVID-19 en una unidad de diálisis domiciliaria (UDD) durante el pico de la pandemia.
Métodosestudio observacional y retrospectivo que incluye todos los pacientes diagnosticados de COVID-19 de la UDD del Hospital Universitario La Paz (Madrid, España) entre el 10 de marzo y el 15 de mayo de 2020. Se recogieron los datos clínicos de la UDD (57 pacientes en diálisis peritoneal [PD] y 22 pacientes en hemodiálisis domiciliaria [HDD]) y comparamos las características clínicas y la evolución de los pacientes con o sin infección por COVID-19.
Resultadosdoce pacientes fueron diagnosticados de COVID-19 (9 DP, 3 HDD). No hubo diferencias estadísticamente significativas entre las características clínicas de los pacientes con COVID-19 y el resto de la unidad. La edad media fue 62 ± 18.5 años; la mayoría eran varones (75%). Todos los pacientes menos uno necesitaron hospitalización. Diez pacientes (83%) fueron dados de alta tras una media de 16,4 ± 9,7 días de hospitalización. Dos pacientes fueron diagnosticados durante su hospitalización por otro motivo y fueron los únicos que fallecieron. Los fallecidos eran de mayor edad que los supervivientes.
ConclusiónLa incidencia de COVID-19 en nuestra UDD en Madrid durante el pico de la pandemia fue alto, especialmente en los pacientes en DP, sin observarse un potencial beneficio para prevenir la infección en los pacientes en diálisis domiciliaria. La edad avanzada y la transmisión nosocomial fueron los principales factores relacionados con peor pronóstico.
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is a new coronavirus that is affecting the entire global population.1 The clinical presentation varies widely, from asymptomatic to severe respiratory distress requiring mechanical ventilation and admission to an Intensive Care Unit (ICU).2 Severe cases are associated with clotting disorders, thromboembolic complications and a systemic inflammation that can lead to multiple organ dysfunction.3,4
In spite of global measures and lockdowns, on 25 May 2020 the incidence of coronavirus disease 2019 (COVID-19) was still rising, with 5,304,772 laboratory-confirmed cases and more than 342,029 deaths worldwide according to the World Health Organisation. The Spanish Ministry of Health had reported 235,000 confirmed COVID-19 cases in Spain and, according to the Coronavirus Resource Centre of Johns Hopkins University, the incidence in Madrid was 1,021.90 cases per 100,000 inhabitants.
SARS-CoV-2 infection affected more frequently to elderly people with comorbidities, and most studies have focused on populations with chronic obstructive pulmonary disease, hypertension or obesity.5 Patients with chronic kidney disease are a vulnerable population, especially those in end-stage renal disease on dialysis. These patients often have many factors associated with increased risk, such as cardiovascular disease, advanced age, intrinsic frailty and an weakened immune system―.6–8 There is little data on the incidence and course of COVID-19 in dialysis patients. Two recent studies in patients treated with in-centre haemodialysis (HD) found different incidences (2.5% in Wuhan9 and 18.8% in Spain10), but there are no data in the home dialysis population. Home dialysis may imply a protective factor as the repeated contact that occurs with in-centre haemodialysis can be avoided.
The aim of this study is to describe the incidence of COVID-19 in a Home Dialysis Unit (HDU) in Madrid, one of the worst-hit areas in Europe, and to assess its course in this group of patients compared with our in-centre dialysis patients.
Patients and methodsStudy designThis is an observational, retrospective study in all patients of the HDU of Hospital Universitario La Paz (Madrid, Spain) diagnosed with COVID-19 between 10 March and 15 May 2020.
Data collectionEpidemiological, clinical, laboratory and radiological data, as well as the treatments received, were obtained from the hospital's electronic registry data system. The routine blood work included complete blood count, coagulation profile with D-dimer, biochemistry with kidney function, liver function, serum ferritin, lactate dehydrogenase, creatinine kinase, troponin I, C-reactive protein and procalcitonin. We collected the data at the time of the patient's arrival in the Emergency Department and at discharge.
All patients received a chest X-ray and/or chest CT to determine the presence of pneumonia, and all received a nasopharyngeal swab in order to perform a reverse transcription polymerase chain reaction (RT-PCR) test to detect the presence of SARS-CoV-2. A definitive diagnosis of COVID-19 was made based on the following criteria: SARS-CoV-2 positivity by RT-PCR and/or radiographic evidence of pneumonia with typical symptoms (dyspnea, fever or cough) and/or suggestive laboratory results (such as lymphopaenia or D-dimer elevation).
Additionally, we compared the demographic and clinical characteristics of HDU patients with and without COVID-19 infection and of patients on in-centre HD and HDU regimens.
Statistical analysisCategorical variables are expressed as percentages. Continuous variables are presented as mean and standard deviation if distributed normally, and otherwise as median and range. Variables normally distributed were studied using the Kolmogorov-Smirnov test. Percentages were compared using Fisher's exact test and means with the Mann–Whitney U test (non-parametric data). Statistical analysis was performed with the IBM SPSS Statistics 24 software programme. The study was approved by the Independent Ethics Committee of the Hospital Universitario La Paz.
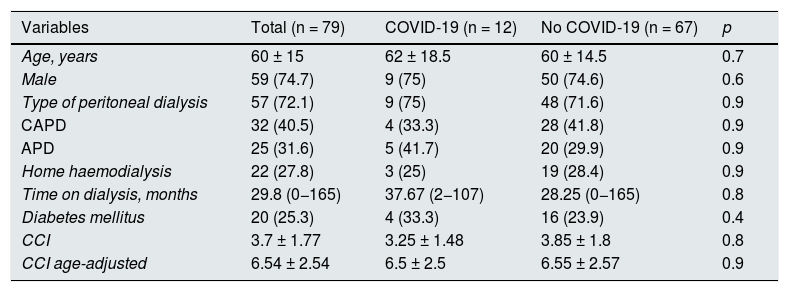
ResultsWe analysed a total of 57 peritoneal dialysis (PD) patients and 22 home haemodialysis (HHD) patients treated in our HDU. Twelve (15.1%) were diagnosed with COVID-19: nine (15.7%) were on PD and three (13.6%) were on HHD. The characteristics of patients with and without COVID-19 are shown in Table 1.
Characteristics of home dialysis patients with and without COVID-19 infection.
| Variables | Total (n = 79) | COVID-19 (n = 12) | No COVID-19 (n = 67) | p |
|---|---|---|---|---|
| Age, years | 60 ± 15 | 62 ± 18.5 | 60 ± 14.5 | 0.7 |
| Male | 59 (74.7) | 9 (75) | 50 (74.6) | 0.6 |
| Type of peritoneal dialysis | 57 (72.1) | 9 (75) | 48 (71.6) | 0.9 |
| CAPD | 32 (40.5) | 4 (33.3) | 28 (41.8) | 0.9 |
| APD | 25 (31.6) | 5 (41.7) | 20 (29.9) | 0.9 |
| Home haemodialysis | 22 (27.8) | 3 (25) | 19 (28.4) | 0.9 |
| Time on dialysis, months | 29.8 (0−165) | 37.67 (2−107) | 28.25 (0−165) | 0.8 |
| Diabetes mellitus | 20 (25.3) | 4 (33.3) | 16 (23.9) | 0.4 |
| CCI | 3.7 ± 1.77 | 3.25 ± 1.48 | 3.85 ± 1.8 | 0.8 |
| CCI age-adjusted | 6.54 ± 2.54 | 6.5 ± 2.5 | 6.55 ± 2.57 | 0.9 |
Data shown as: total number (percentage), mean and standard deviation or median (range).
APD: automated peritoneal dialysis; CAPD: continuous ambulatory peritoneal dialysis; CCI Charlson comorbidity index.
All patients but one were diagnosed as positive for SARS-CoV-2 using the RT-PCR test; the other patient was diagnosed based on clinical, analytical and radiological data. The mean time from onset of symptoms to RT-PCR diagnosis was 7.2 ± 5.7 days (range 0–18). Eleven patient (91.6%) were hospitalised; the patient who did not require hospitalisation was the only one who did not present pneumonia. Two patients were diagnosed during a hospital admission for other reasons (at 3 and 36 days respectively), (nosocomial transmission, 17%).
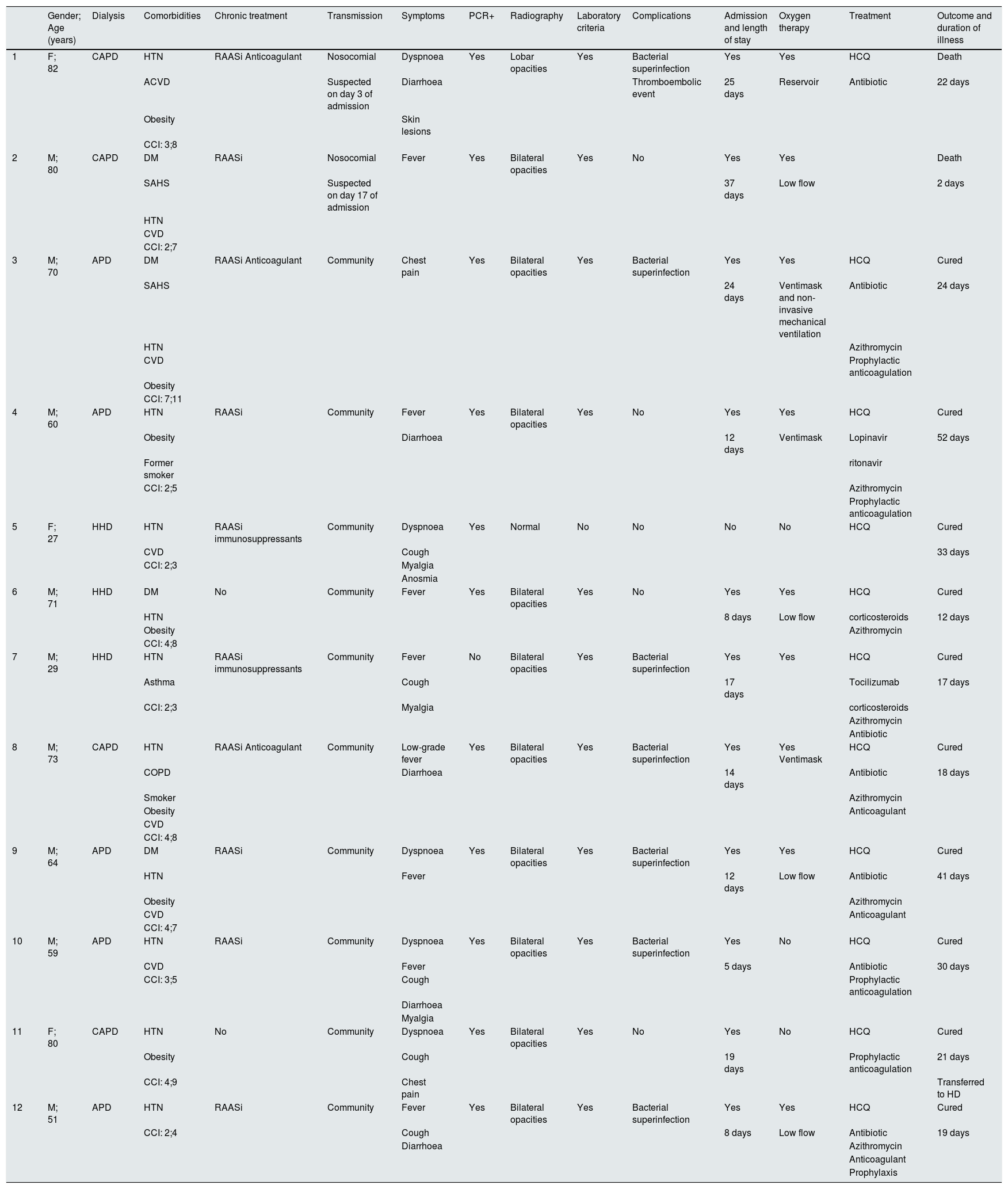
The mean age of the patients was 62 ± 18.5 years (range 27–82); 75% were male, all had hypertension and 33.3% had diabetes. Underlying comorbidities are shown in Table 2. With regard to chronic treatments, 10 patients (83.3%) were using renin-angiotensin-aldosterone system inhibitors, two (16.7%) immunosuppressant treatment and three (25%) anticoagulant treatment.
Clinical characteristics of COVID-19 infection.
| Gender; Age (years) | Dialysis | Comorbidities | Chronic treatment | Transmission | Symptoms | PCR+ | Radiography | Laboratory criteria | Complications | Admission and length of stay | Oxygen therapy | Treatment | Outcome and duration of illness | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F; 82 | CAPD | HTN | RAASi Anticoagulant | Nosocomial | Dyspnoea | Yes | Lobar opacities | Yes | Bacterial superinfection | Yes | Yes | HCQ | Death |
| ACVD | Suspected on day 3 of admission | Diarrhoea | Thromboembolic event | 25 days | Reservoir | Antibiotic | 22 days | |||||||
| Obesity | Skin lesions | |||||||||||||
| CCI: 3;8 | ||||||||||||||
| 2 | M; 80 | CAPD | DM | RAASi | Nosocomial | Fever | Yes | Bilateral opacities | Yes | No | Yes | Yes | Death | |
| SAHS | Suspected on day 17 of admission | 37 days | Low flow | 2 days | ||||||||||
| HTN | ||||||||||||||
| CVD | ||||||||||||||
| CCI: 2;7 | ||||||||||||||
| 3 | M; 70 | APD | DM | RAASi Anticoagulant | Community | Chest pain | Yes | Bilateral opacities | Yes | Bacterial superinfection | Yes | Yes | HCQ | Cured |
| SAHS | 24 days | Ventimask and non-invasive mechanical ventilation | Antibiotic | 24 days | ||||||||||
| HTN | Azithromycin | |||||||||||||
| CVD | Prophylactic anticoagulation | |||||||||||||
| Obesity | ||||||||||||||
| CCI: 7;11 | ||||||||||||||
| 4 | M; 60 | APD | HTN | RAASi | Community | Fever | Yes | Bilateral opacities | Yes | No | Yes | Yes | HCQ | Cured |
| Obesity | Diarrhoea | 12 days | Ventimask | Lopinavir | 52 days | |||||||||
| Former smoker | ritonavir | |||||||||||||
| CCI: 2;5 | Azithromycin | |||||||||||||
| Prophylactic anticoagulation | ||||||||||||||
| 5 | F; 27 | HHD | HTN | RAASi immunosuppressants | Community | Dyspnoea | Yes | Normal | No | No | No | No | HCQ | Cured |
| CVD | Cough | 33 days | ||||||||||||
| CCI: 2;3 | Myalgia | |||||||||||||
| Anosmia | ||||||||||||||
| 6 | M; 71 | HHD | DM | No | Community | Fever | Yes | Bilateral opacities | Yes | No | Yes | Yes | HCQ | Cured |
| HTN | 8 days | Low flow | corticosteroids | 12 days | ||||||||||
| Obesity | Azithromycin | |||||||||||||
| CCI: 4;8 | ||||||||||||||
| 7 | M; 29 | HHD | HTN | RAASi immunosuppressants | Community | Fever | No | Bilateral opacities | Yes | Bacterial superinfection | Yes | Yes | HCQ | Cured |
| Asthma | Cough | 17 days | Tocilizumab | 17 days | ||||||||||
| CCI: 2;3 | Myalgia | corticosteroids | ||||||||||||
| Azithromycin | ||||||||||||||
| Antibiotic | ||||||||||||||
| 8 | M; 73 | CAPD | HTN | RAASi Anticoagulant | Community | Low-grade fever | Yes | Bilateral opacities | Yes | Bacterial superinfection | Yes | Yes Ventimask | HCQ | Cured |
| COPD | Diarrhoea | 14 days | Antibiotic | 18 days | ||||||||||
| Smoker | Azithromycin | |||||||||||||
| Obesity | Anticoagulant | |||||||||||||
| CVD | ||||||||||||||
| CCI: 4;8 | ||||||||||||||
| 9 | M; 64 | APD | DM | RAASi | Community | Dyspnoea | Yes | Bilateral opacities | Yes | Bacterial superinfection | Yes | Yes | HCQ | Cured |
| HTN | Fever | 12 days | Low flow | Antibiotic | 41 days | |||||||||
| Obesity | Azithromycin | |||||||||||||
| CVD | Anticoagulant | |||||||||||||
| CCI: 4;7 | ||||||||||||||
| 10 | M; 59 | APD | HTN | RAASi | Community | Dyspnoea | Yes | Bilateral opacities | Yes | Bacterial superinfection | Yes | No | HCQ | Cured |
| CVD | Fever | 5 days | Antibiotic | 30 days | ||||||||||
| CCI: 3;5 | Cough | Prophylactic anticoagulation | ||||||||||||
| Diarrhoea | ||||||||||||||
| Myalgia | ||||||||||||||
| 11 | F; 80 | CAPD | HTN | No | Community | Dyspnoea | Yes | Bilateral opacities | Yes | No | Yes | No | HCQ | Cured |
| Obesity | Cough | 19 days | Prophylactic anticoagulation | 21 days | ||||||||||
| CCI: 4;9 | Chest pain | Transferred to HD | ||||||||||||
| 12 | M; 51 | APD | HTN | RAASi | Community | Fever | Yes | Bilateral opacities | Yes | Bacterial superinfection | Yes | Yes | HCQ | Cured |
| CCI: 2;4 | Cough | 8 days | Low flow | Antibiotic | 19 days | |||||||||
| Diarrhoea | Azithromycin | |||||||||||||
| Anticoagulant | ||||||||||||||
| Prophylaxis |
APD: automated peritoneal dialysis; CAPD: continuous ambulatory peritoneal dialysis; CCI: Charlson comorbidity index (normal and age-adjusted); COPD: chronic obstructive pulmonary disease; CVD: cardiovascular disease; DM: diabetes mellitus; Duration of illness: time between positive RT-PCR and recovery or death; F: female; HCQ: hydroxychloroquine; HTN: hypertension; M: Male; RAASi: renin-angiotensin-aldosterone system inhibitors; SAHS: sleep apnoea/hypopnoea syndrome.
Table 2 shows the clinical characteristics of COVID-19 infection. Patients' symptoms started at a mean of 5 ± 4.5 days (range 0–13) before hospital admission. Fever was the most frequent symptom (58%), followed by cough (50%). Two patients attended the Emergency Department due to typical chest pain as the main symptom, one of whom had elevated troponin I but no new lesions on coronary angiography, while the other had neither troponin I elevation nor electrocardiographic alterations.
Ten patients (83%) had bilateral lung opacities in imaging tests, one had only unilateral opacities and one did not have pneumonia. The majority (75%) required oxygen therapy, but only one required non-invasive ventilation. Bacterial superinfection was diagnosed in seven patients (58%). All patients presented lymphopaenia, and 88% had high serum D-dimer levels.
Ten patients (83%) were successfully discharged after a mean of 16.4 ± 9.7 days (range 5–37) of hospitalisation. The mean duration from diagnosis to disease resolution was 25.7 ± 11.4 days (range 12–52). One patient was admitted two days to the ICU.
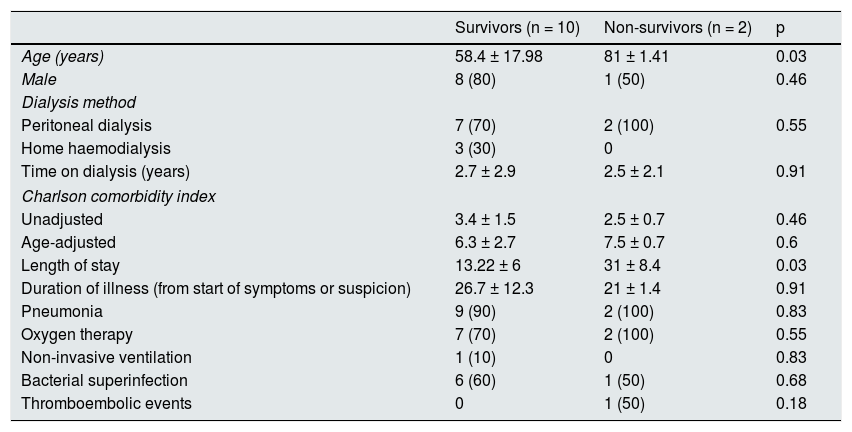
Two PD patients died during the follow-up period, whereas none of the HHD patients died. The overall mortality rate of patients with COVID-19 was 16.6% (22% on PD, 0% on HHD). Global mortality in our HDU was 2.5% (3.5% for PD, 0% for HHD). The two PD patients who died were diagnosed during a hospital admission due to other causes: one was admitted for haemoperitoneum and the other for a myocardial infarction; both developed multiple organ failure. Table 3 shows the differences between COVID-19 survivors and non-survivors. The patients who died were older and with longer hospital admission. No other differences were found between the two groups. After discharge, one PD patient had to be transferred to in-centre HD as they were unable to continue with self-care following the COVID-19 infection.
Comparison between survivors and non-survivors.
| Survivors (n = 10) | Non-survivors (n = 2) | p | |
|---|---|---|---|
| Age (years) | 58.4 ± 17.98 | 81 ± 1.41 | 0.03 |
| Male | 8 (80) | 1 (50) | 0.46 |
| Dialysis method | |||
| Peritoneal dialysis | 7 (70) | 2 (100) | 0.55 |
| Home haemodialysis | 3 (30) | 0 | |
| Time on dialysis (years) | 2.7 ± 2.9 | 2.5 ± 2.1 | 0.91 |
| Charlson comorbidity index | |||
| Unadjusted | 3.4 ± 1.5 | 2.5 ± 0.7 | 0.46 |
| Age-adjusted | 6.3 ± 2.7 | 7.5 ± 0.7 | 0.6 |
| Length of stay | 13.22 ± 6 | 31 ± 8.4 | 0.03 |
| Duration of illness (from start of symptoms or suspicion) | 26.7 ± 12.3 | 21 ± 1.4 | 0.91 |
| Pneumonia | 9 (90) | 2 (100) | 0.83 |
| Oxygen therapy | 7 (70) | 2 (100) | 0.55 |
| Non-invasive ventilation | 1 (10) | 0 | 0.83 |
| Bacterial superinfection | 6 (60) | 1 (50) | 0.68 |
| Thromboembolic events | 0 | 1 (50) | 0.18 |
Data shown as: total number (percentage) or mean and standard deviation.
This study reports COVID-19 incidence and outcomes in an HDU located in one of the most affected areas in Europe. It is difficult to calculate the worldwide incidence of COVID-19 infection in the general population, but on 25 May 2020 there were 10 cases for every 1000 inhabitants in the Madrid region.11 Our cohort includes 12 patients diagnosed with COVID-19, with an overall incidence of 15.1%: nine were on PD (15.7%) and three on HHD (13.6%). There are no pre-existing data on COVID-19 incidence and outcomes in home dialysis patients. Only one study, from Columbia University Irving Medical Center, described 59 COVID-19 patients, two of whom were being treated with PD.12 Several studies have shown the COVID-19 incidence in HD patients, with differing results. A study in Brescia (Italy) reported 21 patients with COVID-19 out of 400 in-centre HD patients, with an incidence of 5.2%,1 while another Italian study found an incidence of 16%.13 Another report, from Wuhan (China), observed an incidence of 16%,14 while a Spanish study in Madrid shows an incidence of 12.7%.2 In our registry of 199 in-centre HD patients, the incidence has been 16.6% (33 patients) during the same period. Several studies report the potential benefit of home dialysis for COVID-19 prevention, as patients may be safer at home, without the need for regular hospital visits.6,15–18 In our area, however, the incidence was similar between home dialysis and in-centre HD patients. These findings may be linked to the high proportion of the population affected in our geographic area. Moreover, community transmission predominated in our HDU.
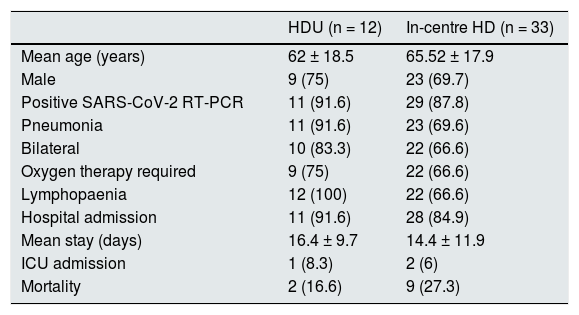
The mean age of our patients with COVID-19 was similar to our hospital's cohort,19 but less than that reported in other HD patients.15 The mean age of our in-centre HD cohort with covid was 65.52 ± 17.9 years. The most common symptoms on admission were fever and cough. These manifestations have also been described as the most common in other studies20 and were also the most common in our in-centre haemodialysis cohort. Two patients were treated in the Emergency Department for chest pain, one of whom had high troponin levels. There are studies that report acute cardiac injury in severe cases of COVID-19 infection.21 In a study conducted in Wuhan (China), five of the first 41 patients with COVID-19 presented myocardial injury with troponin elevation, and their main complaint was cardiac symptoms rather than fever or cough.22 In our cohort, most patients (83%) had bilateral opacities in imaging, similar to those described by Goicoechea et al. in in-centre HD patients.2
Two patients died during follow-up, with an overall COVID-19 mortality rate of 16.6% (PD 22%; HHD 0%). In the general population, the estimated mortality varies between 1.4% and 8%.2 One of the largest COVID-19 case series reported in China found an overall mortality rate of 2.3%23; however, in a study conducted in the New York City area, the mortality rate was 21%.24 In Madrid, the overall mortality rate was 21% up to 25 May11 and 20.7% in our hospital cohort,19 which is higher than that observed in our home dialysis patients. Studies of the HD population have shown greater mortality than in the general population. In Brescia, a mortality rate of 29% has been reported.25 Two Spanish studies with in-centre HD patients found different mortality rates. Albalate et al. reported an overall mortality of 16.2%,10 whereas Goicoechea et al. reported 30.5%.2 A study at Columbia University which included two PD patients had a mortality rate of 31%, but the two PD patients survived.12 In our in-centre HD cohort, mortality was 27.3%. Most studies support the fact that COVID-19 mortality is higher in patients with associated conditions/comorbidities.5 In our cohort, the two patients who died were the oldest, as in the Columbia University study.12 Moreover, both were infected via nosocomial transmission, which indicates that their health status was probably worse than the other affected patients.
Comparison of the clinical characteristics and outcome of patients diagnosed with COVID-19 from our HDU and our in-centre HD cohort are summarised in Table 4. COVID-19 from our HDU had lower frequency of pneumonia, less need for oxygen therapy, lower frequency of lymphopaenia (72.7% vs. 100%) and less need for admission in in-centre HD. By contrast, the overall mortality of the 79 patients in our HDU (2.5%), this is lower than the overall morality of the 199 patients in our in-centre HD cohort (4.5%). A reason to explain this difference could be the epidemiological monitoring protocols used in in-centre HD patients, which could favour early diagnosis and admission of the patients at a less advanced stage of the infection. However due to the limited number of patients in the home dialysis group, it is prudent not to draw any conclusions based on these differences.
Comparison between patients diagnosed with COVID-19 on home dialysis and in-centre HD from our hospital.
| HDU (n = 12) | In-centre HD (n = 33) | |
|---|---|---|
| Mean age (years) | 62 ± 18.5 | 65.52 ± 17.9 |
| Male | 9 (75) | 23 (69.7) |
| Positive SARS-CoV-2 RT-PCR | 11 (91.6) | 29 (87.8) |
| Pneumonia | 11 (91.6) | 23 (69.6) |
| Bilateral | 10 (83.3) | 22 (66.6) |
| Oxygen therapy required | 9 (75) | 22 (66.6) |
| Lymphopaenia | 12 (100) | 22 (66.6) |
| Hospital admission | 11 (91.6) | 28 (84.9) |
| Mean stay (days) | 16.4 ± 9.7 | 14.4 ± 11.9 |
| ICU admission | 1 (8.3) | 2 (6) |
| Mortality | 2 (16.6) | 9 (27.3) |
Data shown as: total number (percentage) or mean and standard deviation.
To our knowledge, this is the first report describing COVID-19 incidence and outcomes in home dialysis patients. These results come from a region with a high incidence of COVID-19 and may not be representative of other areas. All patients had been discharged from hospital when the results were analysed. Nevertheless, our study has a number of limitations. Firstly, the report does not include asymptomatic patients; only those who attended the Emergency Department and the general incidence may have been higher. Secondly, risk factors for mortality could not be analysed due to the low mortality rate observed. Thirdly, due to its retrospective design, some laboratory tests, such as interleukin-6, were not performed in all patients.
In conclusion, the incidence of COVID-19 infection in our home dialysis unit in Madrid during the peak of the pandemic was high, especially in PD patients. The majority of patients required hospitalisation. Advanced age and nosocomial transmission were the main factors linked to a poor prognosis.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We would like to thank the entire team of doctors, nurses, healthcare assistants, porters, cleaners, administrative staff and other personnel of the Hospital Universitario La Paz for their hard work during the COVID-19 pandemic, and in particular their excellent teamwork. We would also like to thank the haemodialysis centre associated with Hospital La Paz (Centro de Diálisis de Madrid El Pilar [Fresenius Medical Care], Centro de Diálisis Alcobendas [Alcobendas Dialysis Centre] [Fresenius Medical Care] and Centro de Diálisis Diaverum Madrid [Diaverum Madrid Dialysis Centre]) for their important role during the pandemic in lending the logistical support necessary to enable all positive COVID-19 cases to be brought together in the hospital unit and healthy patients diverted to the centres.
Please cite this article as: Maldonado M, Ossorio M, del Peso G, Santos-Alonso C, Álvarez L, Sánchez-Villanueva R, et al. Incidencia y resultados de la COVID-19 en una unidad de diálisis domiciliaria en Madrid (España) durante el pico de la pandemia. Nefrologia. 2021;41:329–336.