Hypernatremia is a common electrolyte disorder with increased morbidity and mortality, especially in elderly and critically ill patients. It is most frequently associated with free water losses, but it can also be induced by the administration of hypertonic saline or sodium bicarbonate.1,2 The mortality rates for critically ill patients with hypernatremia are as high as 50%.3 Symptoms from hypernatremia include lethargy, weakness, irritability, seizures, and are as severe as coma.4,5
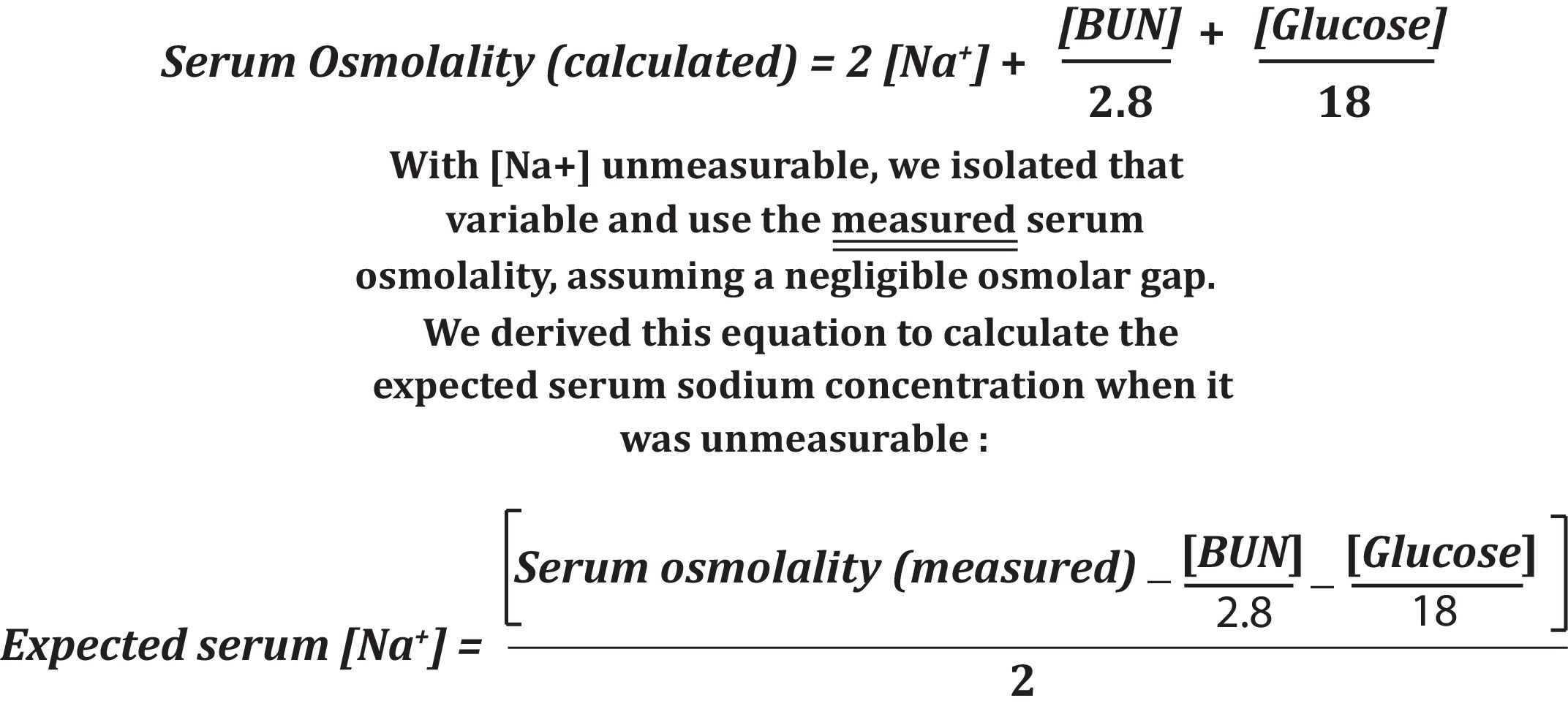
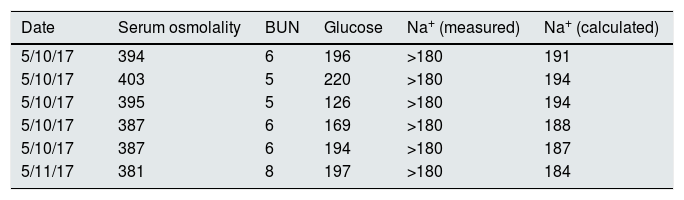
A 59-year-old Caucasian female presented to the hospital with subarachnoid hemorrhage and severe intracranial hypertension (ICH). The patient required intubation for ventilator support, and started on vasopressors for hemodynamic support. She was also started on hypertonic (3%) saline as an adjunctive therapy for her ICH. On admission, her serum sodium was 141mEq/l. Over the next 4 days, despite hypertonic saline having been discontinued, the patient developed severe hypernatremia that was undetectable by the standard assay (ion specific electrode). Her serum sodium was measured as >180mEq/l. She also developed polyuria with a urine osmolality of 220mOsm/l, raising the possibility of diabetes insipidus. D5W was started for this patient in combination with scheduled doses of DDAVP to decrease her serum sodium slowly. We had to use the equation (Fig. 1) for serum osmolality to calculate the serum sodium, given the significantly elevated levels, to ensure proper correction. We recognized that the equation is an indirect marker for serum sodium determination, which incorporates blood urea nitrogen and serum glucose concentrations in its calculation. Her peak serum osmolality was 403mOsm/kg, and it was later lowered to 381mOsm/kg in a 24-h interval (Table 1). It was not until 30h into therapy that the serum sodium level became detectable at 173mEq/l, with a concomitant serum osmolality of 366mOsm/kg.
Lab parameters during hospitalization.
| Date | Serum osmolality | BUN | Glucose | Na+ (measured) | Na+ (calculated) |
|---|---|---|---|---|---|
| 5/10/17 | 394 | 6 | 196 | >180 | 191 |
| 5/10/17 | 403 | 5 | 220 | >180 | 194 |
| 5/10/17 | 395 | 5 | 126 | >180 | 194 |
| 5/10/17 | 387 | 6 | 169 | >180 | 188 |
| 5/10/17 | 387 | 6 | 194 | >180 | 187 |
| 5/11/17 | 381 | 8 | 197 | >180 | 184 |
5/10/17 determinations made during 5h intervals.
In conclusion, using the equation for serum osmolality is an indirect method to calculate the serum sodium level,6 which was especially useful in this patient with severe hypernatremia that was unmeasurable (>180mEq/l) with our standard assay. The applicability of the above mentioned formula allowed us to decreased the patients undetectable serum sodium close to normal range, preventing over-correction and under-correction.7,8 We estimate that the patient's serum sodium could have been as high as 194mEq/l.
Despite these limitations, we were able to indirectly monitor the patient's serum sodium level and adequately correct to goal.9,10 The patient survived her hospitalization and was discharged to a rehabilitation unit with improved serum sodium levels.