In membranous nephropathy, the presence of antibodies against M-type phospholipase A2 receptor is considered highly specific for idiopathic forms. However, no specific association to a particular clinical profile has been found for such antibodies.
ObjectiveTo assess potential differences in initial clinical profile, course and prognosis of idiopathic membranous nephropathy depending on the presence of anti-PLA2R antibodies.
MethodsEighty-five patients with idiopathic membranous nephropathy were included (55 anti-PLA2R-positive and 30 anti-PLA2R-negative). Clinical, biochemical and pathological variables were recorded at the time of diagnosis. Frequency of spontaneous remission, incidence of response to first-line therapy, frequency and number of recurrences, survival of renal function free from renal replacement therapy, survival of renal function free from chronic renal insufficiency and frequency of occurrence of malignant, infectious or autoimmune diseases during follow-up were recorded.
ResultsAt the time of diagnosis, anti-PLA2R-negative patients were significantly older and had a higher frequency of spontaneous remission. No differences were noted in the response to first-line treatment, frequency and number of recurrences, survival of renal function free from renal replacement therapy, or survival of renal function free from chronic renal insufficiency.
ConclusionsAnti-PLA2R-negative patients with idiopathic membranous nephropathy were older and experienced spontaneous remission more often than anti-PLA2R-positive patients. No differences in terms of treatment response, recurrences, and final prognosis were observed between both groups of patients.
En la nefropatía membranosa (NM), la presencia de anticuerpos antirreceptor tipo M de fosfolipasa A2 se considera altamente específica para las formas idiopáticas, pero no se ha demostrado que la presencia de dichos anticuerpos se asocie a un determinado perfil clínico.
ObjetivoAnalizar si existe alguna diferencia en cuanto al perfil clínico inicial, evolución y pronóstico entre pacientes con NM idiopática en función de la presencia de anticuerpos anti-PLA2R.
MétodosSe estudió a 85 enfermos con NM idiopática, 55 eran anti-PLA2R positivos y 30 negativos. Se registraron las variables clínicas, bioquímicas y anatomopatológicas al momento del diagnóstico, la frecuencia de remisión espontánea, la incidencia de respuesta al tratamiento de primera línea, la frecuencia y número de recidivas, la supervivencia de la función renal libre de tratamiento sustitutivo renal, la supervivencia de la función renal libre de insuficiencia renal crónica y la frecuencia de aparición de enfermedades neoplásicas, infecciosas o autoinmunes durante el seguimiento.
ResultadosAl momento del diagnóstico, los enfermos anti-PLA2R negativos presentaron significativamente mayor edad y frecuencia de remisión espontánea. No se apreciaron diferencias en la respuesta al tratamiento de primera línea, frecuencia ni número de recidivas, supervivencia de la función renal libre de tratamiento sustitutivo renal ni supervivencia de función renal libre de insuficiencia renal crónica.
ConclusionesLos enfermos con NM idiopática anti-PLA2R negativos presentaron mayor edad, menor filtrado glomerular inicial y mayor frecuencia de remisión espontánea que los enfermos anti-PLA2R positivos. Sin embargo, entre ambos grupos de enfermos, no se observaron diferencias en cuanto a la respuesta y al tratamiento, aparición de recidivas ni pronóstico final.
Membranous nephropathy (MN) is the leading cause of nephrotic syndrome among adults.1 It is clinically classified into idiopathic (IMN) or secondary, depending on the identification of an aetiology. When clinical or biochemical data suggesting a specific cause are not available, their differentiation based on the sole use of data derived from renal biopsies can be challenging.2,3 Several recent studies have reported that nearly 70% of IMN cases are associated with the presence of antibodies against M-type phospholipase A2 receptor (anti-PLA2R).4 The likelihood of spontaneous remission5 (SR) and treatment response is associated with antibody titres at diagnosis.5–10 Nonetheless, the presence of anti-PLA2R antibodies in IMN patients was not shown to be associated with a particular clinical profile or to result in differences regarding clinical course, treatment response, or long-term prognosis. Also, and despite the majority of trials agreeing that the presence of anti-PLA2R antibodies is highly specific for idiopathic forms of MN,4,5,7,12–14 the said antibodies have been reported to be consistent with other potential aetiologies,15 and around 30% of IMN patients are anti-PLA2R negative. Antibodies against other podocyte antigens whose clinical correlation is still under investigation have been described in this last group of patients,16–19 which is why the potential identification of secondary aetiologies over time remains largely uncertain. Yet, given that most trials had a transversal design, little information is available on the diagnosis of potential aetiologies of MN over time in anti-PLA2R positive and negative patients.
The purpose of this study is to assess potential differences in initial clinical profile, clinical course, treatment response, or prognosis of IMN based on the presence or absence of anti-PLA2R antibodies.
Patients and methodsWe conducted a retrospective study involving patients over 18 years old with a renal biopsy diagnosis of nephrotic syndrome secondary to MN between 1985 and 2009, who complied with the following criteria: (1) absence of an aetiology of MN, following a protocol study which ruled out neoplastic, systemic, and infectious diseases or exposure to drugs at diagnosis, and (2) available renal tissue samples for immunohistochemistry or serum samples at diagnosis for the measurement of circulating anti-PLA2R antibodies.
Clinical, demographic, and biochemical variables were recorded at the time of diagnosis and during follow-up. Serum creatinine was determined using a compensated IDMS-traceable method (Hitachi Modular P-800 Roche Diagnostics, Berlin, Germany). The estimated glomerular filtration rate (eGFR) was measured using CKD-EPI.20
Patients were classified into two groups based on the presence or absence of anti-PLA2R antibodies shown by immunohistochemistry in the renal biopsy or by the evidence of high circulating levels at diagnosis.
The percentage of glomerular sclerosis was determined in all renal biopsies, together with the extent of interstitial fibrotic lesions, which was classified into four categories: 0: absent; grade I: ≤25%; grade II: 26–50%, and grade III: >50%. For biopsies where paraffin-embedded specimens were available, 5μm sections were made for anti-PLA2R antibody staining (HPA012657 Sigma–Aldrich Co. LLC, Munich, Germany) by immunohistochemistry (IHC) based on the previously described technique.13
Circulating anti-PLA2R antibodies were measured using ELISA (Euroimmun, Lübeck, Germany; linearity: 6–1500RU/mL; lowest detection limit: 0.6RU/mL). Titres ≥20RU/mL were considered positive.
Follow-up and controlsFollowing diagnosis, all patients underwent follow-up and observation prior to initiation of immunosuppression, during which symptomatic treatment was prescribed, including a low-sodium diet, and patients diagnosed from 1994 onwards received angiotensin receptor blockers and statins. Patients who did not achieve SR following observation received immunosuppressants.
Outcome measures(1) Percentage and incidence of SR. (2) Incidence of response (total or partial remission) in the 12 months following first-line treatment initiation. (3) Time between treatment initiation and remission. (4) Percentage of patients experiencing recurrences, incidence and total number of recurrences. (5) Survival of renal function free from renal replacement therapy at the end of follow-up. (6) Survival of renal function free from chronic renal failure (CRF) at the end of follow-up. (7) Frequency of development of de novo neoplasia or other potential causes for MN during observation.
DefinitionsComplete remission: proteinuria <0.3g/day in two consecutive controls. Partial remission: proteinuria <3.5g/day, and >0.3g/day in two consecutive controls. SR: complete or partial remission without immunosuppressants. Recurrence: proteinuria >3.5g/day associated with hypoalbuminaemia in two consecutive controls following treatment suppression. CRF: eGFR <60mL/min/1.73m2.
The trial complied with the Helsinki Declaration parameters and was approved by the centre's Bioethics Committee.
Statistical analysisResults are summarised as mean and typical deviation for normal distribution variables or as median and interquartile ranges for skewed distribution variables. Mean differences between study groups were analysed using Student's t test for independent data or Mann–Whitney U test. A variance analysis (ANOVA) was used for differences between more than two means. Ratio differences were analysed using Chi-square test or Fisher exact test. Independent predictors of SR were analysed using a stepwise logistic regression model. The discriminatory capacity was analysed using area under the ROC curve, and risk calibration was assessed through the Hosmer–Lemeshow test.21 Independent variables associated with remission rates following treatment and overall survival of renal function at the end of follow-up were analysed using Kaplan–Meier estimates with the log-rank test for group differentiation, followed by Cox regression analysis to identify independent predictors. All p<0.05 values were considered statistically significant. The statistical program SPSS v. 20.0 was used.
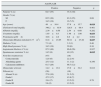
ResultsTable 1 summarises the clinical, biochemical, and pathological characteristics of the 85 patients enrolled in the study, based on the presence or absence of anti-PLA2R antibodies. The anti-PLA2R positive study group consisted of 55 patients: 15 (27.1%) had high titres of anti-PLA2R antibodies detected through ELISA, while immunohistochemistry was not possible owing to the absence of sufficient biopsy material; glomerular deposition was detected in 10 patients (17.6%) by immunohistochemistry, though no serum sample was available to determine antibody titres at diagnosis, and 30 (54.5%) patients had positive antibodies in both serum and renal biopsy.
Baseline clinical and pathological features of patients based on the presence or absence of anti-PLA2R antibodies.
| Anti-PLA2R | |||
|---|---|---|---|
| Positive | Negative | p | |
| Patients % (n) | 64.7 (55) | 35.3 (30) | |
| Gender % (n) | |||
| M | 65.5 (36) | 83.3 (25) | 0.08 |
| F | 34.5 (19) | 16.7 (5) | |
| Age (years) | 49±16.4 | 57.8±15.7 | 0.019 |
| Cholesterol total (mg/dL) | 340.2±85.9 | 326.5±68.4 | 0.461 |
| Albumin (mg/dL) | 2.39±0.56 | 2.54±0.68 | 0.282 |
| Creatinine (mg/dL) | 1.03±0.3 | 1.48±1.08 | 0.033 |
| Proteinuria (g/24h) | 10.6±4.6 | 8.6±4.2 | 0.064 |
| Glomerular filtration (mL/min/1.73m2) | 81.8±23.65 | 69.11±27.28 | 0.027 |
| Diabetes % (n) | 7.3 (4) | 3.3 (1) | 0.46 |
| High blood pressure % (n) | 34.5 (19) | 20 (6) | 0.16 |
| Angiotensin blockers ii % (n) | 87.2 (48) | 86.6 (26) | 0.937 |
| Spontaneous remission % (n) | 14.5 (8) | 40 (12) | 0.015 |
| First-line treatment (n) | (47) | (18) | |
| Corticosteroids | 12.8 (6) | 22.2 (4) | |
| Alkylating agents | 25.5 (12) | 11.1 (2) | 0.356 |
| Calcineurin inhibitors | 61.7 (29) | 66.7 (12) | |
| Glomerular sclerosis | 14.2±19.1 | 15.9±32.2 | 0.812 |
| Fibrosis (n) | (36) | (16) | |
| Absent % (n) | 27.8 (10) | 31.2 (5) | |
| Grade I | 47.2 (17) | 43.8 (7) | |
| Grade II | 19.4 (7) | 12.5 (2) | 0.78 |
| Grade III | 5.6 (2) | 12.5 (2) | |
Only p values under 0.05 are highlighted in bold.
Anti-PLA2R positive patients were significantly younger (p: 0.019), had lower creatinine levels and higher eGFR compared to anti-PLA2R negative patients (p: 0.033 and 0.027, respectively). When analysing baseline creatinine distribution in the two groups, three anti-PLA2R negative patients had exceptionally high creatinine levels compared to the rest of the group. No significant differences were observed between anti-PLA2R positive and negative patients after these patients were excluded from analysis. No differences were observed in the remaining clinical and pathological variables under study.
Mean observation time prior to treatment was 8.34±6.25 months (median: 6.5; P25: 6 and P75: 9 months). A total of 20 patients (23.5%) achieved SR. The incidence of SR was of 0.041 episodes/patient/month. In the univariate analysis, SR was associated with lower proteinuria at baseline (6.84±3.10 vs 10.88±4.53g/24h; p<0.001), higher albuminaemia (2.82±0.65 vs 2.32±0.54g/dL; p: 0.001), and anti-PLA2R negativity (SR: 12/30 [40%] anti-PLA2R negative vs 8/55 [14.5%] in anti-PLA2R positive; p: 0.015). In the multivariate analysis, proteinuria and anti-PLA2R negativity were the single SR-independent predictors (Table 2). No significant differences were reported in time to SR among anti-PLA2R positive and negative patients (7.10±2.60 vs 7.28±2.42 months; p: 0.893). No association between baseline antibody titres and frequency of SR was observed in the 45 patients with anti-PLA2R antibody titre values.
Immunosuppressants were administered to the 65 patients who did not achieve SR. Ten patients (15.6%) received prednisone alone, 14 (21.8%) received alkylating drugs (cyclophosphamide or chlorambucil) in combination with corticosteroids for 6 months, and 41 (63%) were treated with calcineurin inhibitors (cyclosporine or tacrolimus) for at least 6 months and a maximum of 12 months. No significant differences were reported in terms of kind of drug used as first-line therapy among anti-PLA2R positive and negative patients. Three (30%) of the 10 patients receiving corticosteroids alone achieved partial remission in the 12 months following treatment initiation. Two of them experienced recurrence. One received treatment with cyclophosphamide and achieved partial remission; the other received corticosteroids alone again and achieved partial remission. The remaining seven patients only received symptomatic treatment. At the end of follow-up, 6 of the 10 patients treated with corticosteroids (60%) developed CRF, but none progressed to stage V CRD.
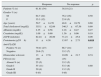
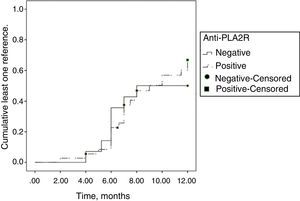
After exclusion of patients receiving steroids alone from the analysis of treatment response, 34/55 patients (61.81%) achieved partial or total remission and 21/55 (38.18%) did not achieve a response. Table 3 summarises the clinical, biochemical, and pathological characteristics of patients based on the assessment of response to first-line treatment at 12 months from baseline. Remission was associated with lower baseline proteinuria. No significant association was reported between any of the remaining variables and baseline treatment response in the first 12 months. The incidence of remission in the first 12 months was similar among anti-PLA2R positive and negative patients (Fig. 1; p: 0.780). No differences were noted among patients receiving alkylating drugs or calcineurin inhibitors (p: 0.40).
Baseline clinical and pathological features of patients based on first-line treatment response.
| Response | No response | p | |
|---|---|---|---|
| Patients % (n) | 61.81 (34) | 38.18 (21) | |
| Gender % (n) | |||
| M | 64.7 (22) | 76.2 (16) | 0.50 |
| F | 35.3 (12) | 23.8 (5) | |
| Age (years) | 50.7±14.70 | 48.8±18.79 | 0.69 |
| Total cholesterol (mg/dL) | 355.1±82.09 | 346.5±67.56 | 0.69 |
| Albumin (mg/dL) | 2.35±0.58 | 2.18±0.47 | 0.27 |
| Creatinine (mg/dL) | 1.09±0.60 | 1.36±0.96 | 0.19 |
| eGFR (mL/min) | 82.24±26.89 | 71.21±25.8 | 0.09 |
| Proteinuria (g/24h) | 11±4.38 | 13.67±2.73 | 0.018 |
| Anti-PLA2R | |||
| Positive % (n) | 79.41 (27) | 66.7 (14) | 0.37 |
| Negative | 20.6 (7) | 33.3 (7) | |
| Glomerular sclerosis | 13±17.6 | 10.99±21.7 | 0.74 |
| Fibrosis (n) | (20) | (15) | |
| Absent % (n) | 25 (5) | 33.3 (5) | |
| Grade I | 55 (11) | 53.3 (8) | 0.80 |
| Grade II | 20 (4) | 13.3 (2) | |
| Grade III | 0 (0) | 0 (0) | |
Total cholesterol: mean total cholesterolaemia.
Alternative immunosuppressants were administered to the 21 non-responders to first-line treatment. A total of nine (90.47%) patients received calcineurin inhibitors and two (9.52%) patients received calcineurin inhibitor plus rituximab, with total or partial remission observed in all cases.
Mean follow-up was 75.3±49 months (median: 62; P25: 39; P75: 105 months). During this time, 32 of the 54 remitting patients (59.2%) experienced recurrence, including 6 of the 20 patients achieving SR (30%) and 26 of the 34 patients with post-treatment remission (76.4%). Mean recurrences were of 1.59±1.25 (interval 0–5). The incidence of recurrences was 0.033 episodes/patient/year. No statistically significant differences were reported between the frequency or incidence of recurrences and any of the study variables. No significant differences were reported in the number of recurrences between anti-PLA2R positive (1.32±0.56) and negative (1.94±1.74; p: 0.07) patients. The number of recurrences between patients receiving calcineurin inhibitors and patients receiving alkylating agents as first-line treatment was not significant either.
Twenty-six (81.2%) patients experiencing recurrence received calcineurin inhibitors and six (18.8%) received alkylating agents, achieving total or partial remission of the nephrotic syndrome in 93.7% of cases (n: 30). Calcineurin inhibitors were continued for a mean time of 47.8±20.8 months (range 22–83) in ten patients experiencing more than three recurrences. These patients were subsequently treated with rituximab, achieving calcineurin inhibitor treatment suppression for all cases.22
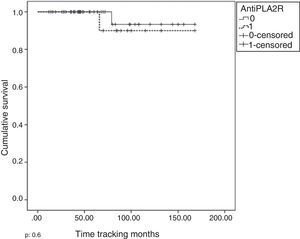
At the end of follow-up, survival of renal function free from renal replacement therapy was 95.2%. Fig. 2 illustrates the survival of renal function free from renal replacement based on the presence or absence of anti-PLA2R antibodies. No significant differences were seen between groups. CRF-free survival of renal function was 70%. Table 4 summarises the variables associated with the development of CRF in the univariate (A) and multivariate (B) analyses. In this group, age, baseline renal function, and evidence of remission within the first year of immunosuppressive treatment were the single independent predictors of RF development.
CRD-associated variables in the univariate (A) and multivariate (B) analysis.
| (A) | CRF | Without CRF | p |
|---|---|---|---|
| Patient % (n) | 31.08 (23) | 68.91 (51) | |
| Age | 62.65±17.052 | 47.12±13.85 | <0.001 |
| Baseline eGFR (mL/min) | 59.91±24.8 | 68.19±21.12 | <0.001 |
| ACE treatment % (n) | 82.6 (19) | 100 (51) | 0.008 |
| HBP % | 56.5 (13) | 23.5 (12) | 0.008 |
| Glomerular sclerosis % | 23.05±28.63 | 8.78±15.97 | 0.039 |
| Fibrosis (n) | (17) | (27) | |
| Absent % (n) | 11.8 (2) | 40.7 (11) | |
| Grade I | 35.3 (6) | 51.9 (14) | <0.001 |
| Grade II | 41.2 (7) | 7.4 (2) | |
| Grade III | 11.8 (2) | 0 (0) | |
| Remission in the first 12 months following start of treatment % (n) | 30.8 (4) | 73.2 (30) | 0.009 |
| (B) | B | Wald | OR | CI (95%) | p |
|---|---|---|---|---|---|
| Age | 0.083 | 6.172 | 1.087 | 1.018–1.161 | 0.013 |
| Baseline eGFR | −0.05 | 7.558 | 0.95 | 0.918–0.986 | 0.006 |
| Remission in the 12 months from start of immuno-suppression % (n) | −2.90 | 4.37 | 0.055 | 0.004–0.834 | 0.036 |
Two patients, one anti-PLA2R positive, the other anti-PLA2R negative, developed de novo neoplasia during follow-up, both consistent with prostate adenocarcinomas. The time between diagnosis of MN and neoplasia was 3.5 years. An anti-PLA2R negative male patient under partial remission died during follow-up from an acute coronary syndrome 48 months after diagnosis of MN.
DiscussionOur data reveal that IMN patients show similar biochemical and pathological profile at diagnosis – except for age – irrespective of the presence of anti-PLA2R antibodies. The likelihood of SR was significantly higher among anti-PLA2R negative patients after adjusting for proteinuria and baseline renal function. These data are consistent with those in a number of recent studies,14 though in disagreement with others7,11, and show no significant differences between anti-PLA2R positive and negative patients. The frequency of SR was slightly lower than that described in previous trials23–25 and, unlike these previous reports, no association was identified between renin-angiotensin-aldosterone blockers and baseline renal function. The absence of a link to the use of angiotensin II blockers may be explained by the fact that most patients diagnosed before 1994 had not been systematically prescribed with this type of drug following diagnosis. In addition, this fact could also partly account for the lower frequency of SR as reported in our cohort. Additionally, given that the frequency of SR increases over time,25 longer observation periods might have resulted in increased frequency. The absence of a link to baseline renal function may be explained by normal renal function of most patients at baseline. Mean baseline creatinine and eGFR were lower among anti-PLA2R negative patients. The possibility of ST would be expected to be lower in this group. However, this was not observed in the univariate and multivariate analyses. The reason here lies in the fact that three patients from this group had extreme creatinine levels, which influenced the size of the mean values. Following exclusion from analysis, and after the comparison, no significant differences were observed. Anti-PLA2R negativity behaved as an independent variable and was associated with a higher probability of SR. These results may suggest that observation time prior to active immunosuppression can be extended in anti-PLA2R negative IMN patients, provided there is no exacerbation of renal function or proteinuria. Nevertheless, this finding must be confirmed by other trials before the suggestion can be considered conclusive.
Post-treatment outcome, first-line treatment response, recurrences, and renal function survival rate were similar between anti-PLA2R positive and negative patients. These data are consistent with other recent studies already published.7,9,10,23 The presence of anti-PLA2R antibodies in the multivariate analysis was not an independent predictor of long-term survival of renal function.
One last finding from our data is that no potential IMN-related diseases were diagnosed after extended follow-up in any of the patients initially diagnosed with IMN, irrespective of the presence or absence of anti-PLA2R antibodies, showing that the probability of a secondary aetiology is low, in both anti-PLA2R positive and negative patients, unless otherwise revealed at diagnosis.
Our study is based on a retrospective cohort, and as such faces certain limitations and may be biased as a result of the influence of unmeasured variables. First, although the presence of anti-PLA2R antibodies in all patients classified as having positive anti-PLA2R antibodies is certain, they should have been identified through the combination of immunohistochemical and serological techniques, as the two sets of information were not concurrently available in some patients. Consequently, only partial analysis of the association between anti-PLA2R titres and the probability of SR was possible, thus affecting the statistical power of the results. Second, the study includes patients diagnosed and treated over a very long period, when study protocols, follow-up, and treatments differed and were not always governed by clearly defined guidelines. Although an analysis consistent with real clinical practice at each time point is possible, comparison of the data is therefore difficult, which might explain some of the differences found with other groups of patients in the literature, where decisions were made based on protocol- or guideline-defined criteria. Of note, 10 of the 64 patients without SR received corticosteroids alone. All had been treated before this treatment was shown in various studies to be ineffective in changing the clinical course of IMN. For this reason their progress is described separately, following exclusion from the efficacy analysis in terms of first-line treatment response.
In conclusion, our data show that patients with IMN associated to anti-PLA2R antibodies are older at diagnosis and their frequency of SR is higher than that of anti-PLA2R positive patients. However, no differences between the two groups of patients were found in terms of response to first-line treatment, time to remission, frequency and number of recurrences, diagnosis of potential MN-related causes, and prognosis following observation.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Jatem Escalante E, Segarra Medrano A, Carnicer Cáceres C, Martín-Gómez MA, Salcedo Allende MT, Ostos Roldan H, et al. Características clínicas, evolución y pronóstico de la nefropatía membranosa idiopática en función de la presencia de anticuerpos contra el receptor tipo M de la fosfolipasa A2. Nefrologia. 2015;35:479–486.