Debido a los movimientos poblacionales que se desarrollan actualmente, existe un incremento en el número de individuos con enfermedad de Chagas (EC) que viven en regiones no endémicas; por tanto, existe una gran probabilidad de que nos enfrentemos a un aumento de casos de EC, tanto en pacientes que requieren tratamiento renal sustitutivo como en potenciales donantes. Presentamos el caso de un donante de órganos con serología Trypanosoma cruzi positiva, cuyos riñones se implantaron en sendos receptores. Se realizó profilaxis con benznidazol durante 3 semanas. En dos años de seguimiento serológico y clínico no se ha objetivado ninguna evidencia de transmisión ni afectación chagásica. La buena evolución sugiere que el trasplante de riñones procedentes de donantes con serología positiva sin signos de enfermedad aguda o crónica puede ser aceptable. Revisamos las evidencias que lo sustentan y las recomendaciones disponibles en la literatura.
Due to current trends in human population movements, there has been an increase in the number of individuals with Chagas’ disease (CD) living in non-endemic regions; as such, there is a high probability that we will face an increase in cases of CD, both in patients requiring renal replacement therapy and in potential donors. We present the case of an organ donor with positive serology for Trypanosoma cruzi, whose kidneys were implanted into two different recipients. Prophylaxis was administered with benznidazole for 3 weeks. Over the course of two years of serological and clinical follow-up, no evidence of Chagas’ transmission or infection was observed. This positive evolution suggests that renal transplants derived from donors with positive serology results and no signs of acute or chronic disease may be acceptable. We also provide a review of the evidence supporting this conclusion and the available recommendations in the medical literature.
INTRODUCTION
Chagas’ disease (CD) is an uncommon entity in Spain, but it does have a high prevalence in South America. It is produced by infection from Trypanosoma cruzi, an intracellular parasite that is transmitted to humans through bites from haematophagous insects, blood transfusion, vertical transmission, and less frequently, through organ transplantation. Following transmission, the parasite lodges inside the host cells where it multiplies (amastigote). Later, following cell rupture, T. cruzi is disseminated throughout the bloodstream in the form of a trypoamastigote. Once in the circulatory system, any cell in the body can be infected except for neurons.1 The disease first develops as an acute phase with elevated parasitemia, which in 95% of cases is asymptomatic. In symptomatic cases, the only clinical signs involve non-specific fever. Two-thirds of all infected patients then enter into an indeterminate phase, in which they may remain for decades. This phase is also characterised as being asymptomatic, but with positive serology test results. All other patients develop symptoms of chronic CD, usually characterised by cardiomyopathy, which is the primary cause of death.2 Another common form of clinical presentation are “megasyndroms”, which include megacolon and mega-oesophagus.1
The diagnosis of CD relies on detection of the parasite in the bloodstream during the acute phase, or through serological tests (primarily ELISA) during acute, indeterminate, and chronic disease phases. Diagnosis using PCR was standardised in 2010, but the World Health Organisation (WHO) recommended performing at least 2 serological tests for diagnosis3 and using PCR for confirmation in cases of positive results or discrepancies in the results produced by the two tests. Nifurtimox and benznidazole are the most commonly used drugs for the treatment of CD, with a parasitological cure rate of approximately 60% in cases of acute infection.4 Current indications for treatment include acute forms or reactivation of disease, congenital CD, and chronic CD in individuals younger than 18 years of age. Treatment in adults appears to delay the progression of myocardial damage, but not cure it.5 As such, in adults with CD but with no developed cardiomyopathy, the indication for pharmacological treatment must be made on an individual basis, with special emphasis on women at reproductive age or before immunosuppression.
Due to current trends in population movements, there is a growing number of individuals with CD who live in non-endemic regions, and as such, there is a high possibility that we will begin to see an increase in the number of CD cases, both in patients who require renal replacement therapy and those who are potential donors.6
CLINICAL EXPERIENCE
Donor
A female patient of 40 years of age who was originally from Paraguay and who had recently been diagnosed with arterial hypertension (AHT), under treatment suffered brain haemorrhage and was pronounced brain dead. The patient had positive serology for CD, with no manifestations of acute clinical symptoms or chronic disease. The absence of signs and symptoms of CD led to classification of the patient as a potential donor for kidney transplantation.
Recipient 1
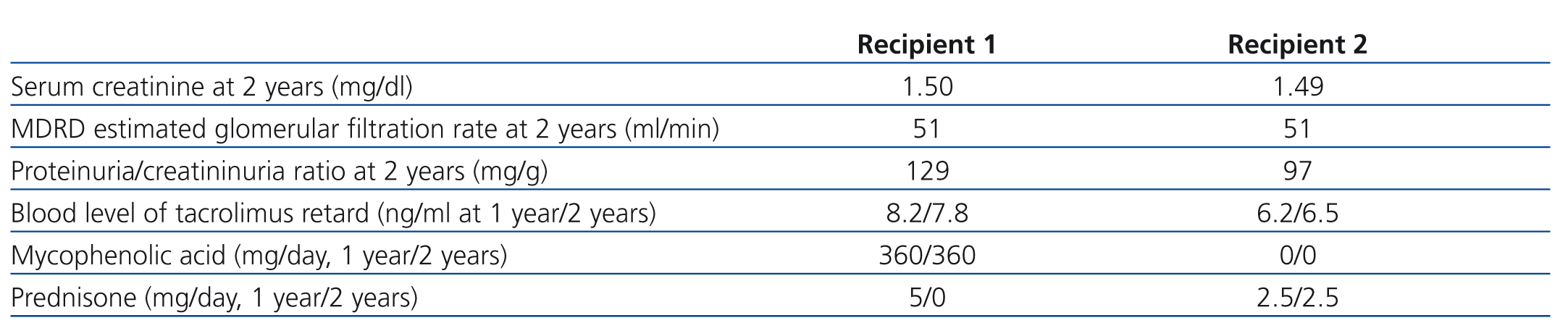
A 51-year-old male with IgA nephropathy was diagnosed as an incidental finding of microhaematuria and proteinuria. The patient started peritoneal dialysis 2 years after diagnosis. He received a kidney transplant (KT) from the aforementioned donor 1 year after having started dialysis. Donor and recipient shared an HLA-B and a DR, the cross-match test was negative, and immunosuppression was based on induction therapy with basiliximab and maintenance therapy with tacrolimus retard, prednisone, and mycophenolic acid. Diuresis commenced immediately, and the patient was discharged with no complications. In the immediate post-transplant period, the patient received benznidazole for prophylaxis at 175mg/12 hours for 3 weeks. We detected no secondary side effects of the drug: haemoglobin was stable, no leuko-thrombocytopenia, and no cutaneous, gastrointestinal, or neurological abnormalities. The evolution of renal function and immunosuppressant therapy is summarised in Table 1. One month after KT, the patient developed obstructive symptoms secondary to lymphocele, which were resolved through marsupialisation. Six months after KT, during an evaluation of poorly controlled AHT, we detected a significant stenosis of the graft’s renal artery, requiring angioplasty with dilation and stent placement. None of these complications were related to CD. We monitored the patient for possible CD transmission through periodical serological tests using ELISA and indirect immunofluorescence every 15 days for the first month, every month for the first year, and then every 6 months for 2 years. All evaluations resulted negative. During these 2 years, we also failed to detect any clinical alterations compatible with acute or chronic CD.
Recipient 2
The second recipient was a 58-year-old male with a history of properly controlled AHT and no complications. The patient had a single kidney as a congenital condition. During evaluation of nephrotic range proteinuria, the patient was diagnosed with focal segmental glomerulonephritis requiring haemodialysis. Eight months later, the patient received a kidney transplant from the aforementioned donor. They shared one HLA-B, and the cross-match test was negative. Conventional immunosuppression was provided in the form of induction therapy with basiliximab and maintenance with tacrolimus retard, prednisone, and mycophenolic acid. We observed delayed graft functioning requiring a single session of haemodialysis. The evolution of renal function and immunosuppression treatment 1 and 2 years after KT are summarised in Table 1. The patient developed pneumonia due to type A influenza 3 weeks following the KT, which necessitated suspending mycophenolic acid (which was never reinstated). Six months after the KT, the patient was diagnosed with a cutaneous fungal infection on the left leg from Alternaria alternata. We administered oral voriconazole treatment, which resolved the infection. Two years after KT, altered hepatic biochemical parameters led to an evaluation, and the patient was diagnosed with hepatocellular carcinoma of a cirrhotic liver secondary to non-alcoholic steatohepatitis. At this point, the patient continues to receive treatment and evaluations with intent to cure this carcinoma. There is no evidence in the medical literature to relate CD with the development of neoplastic disease. The protocol for monitoring and providing prophylaxis for CD was the same as in the first case. Prophylaxis has been well tolerated both in terms of clinical response and laboratory parameters. All serological tests have resulted negative. No symptoms indicative of CD have been reported, nor have any echocardiographic or electrocardiographic abnormalities been observed.
REVIEW
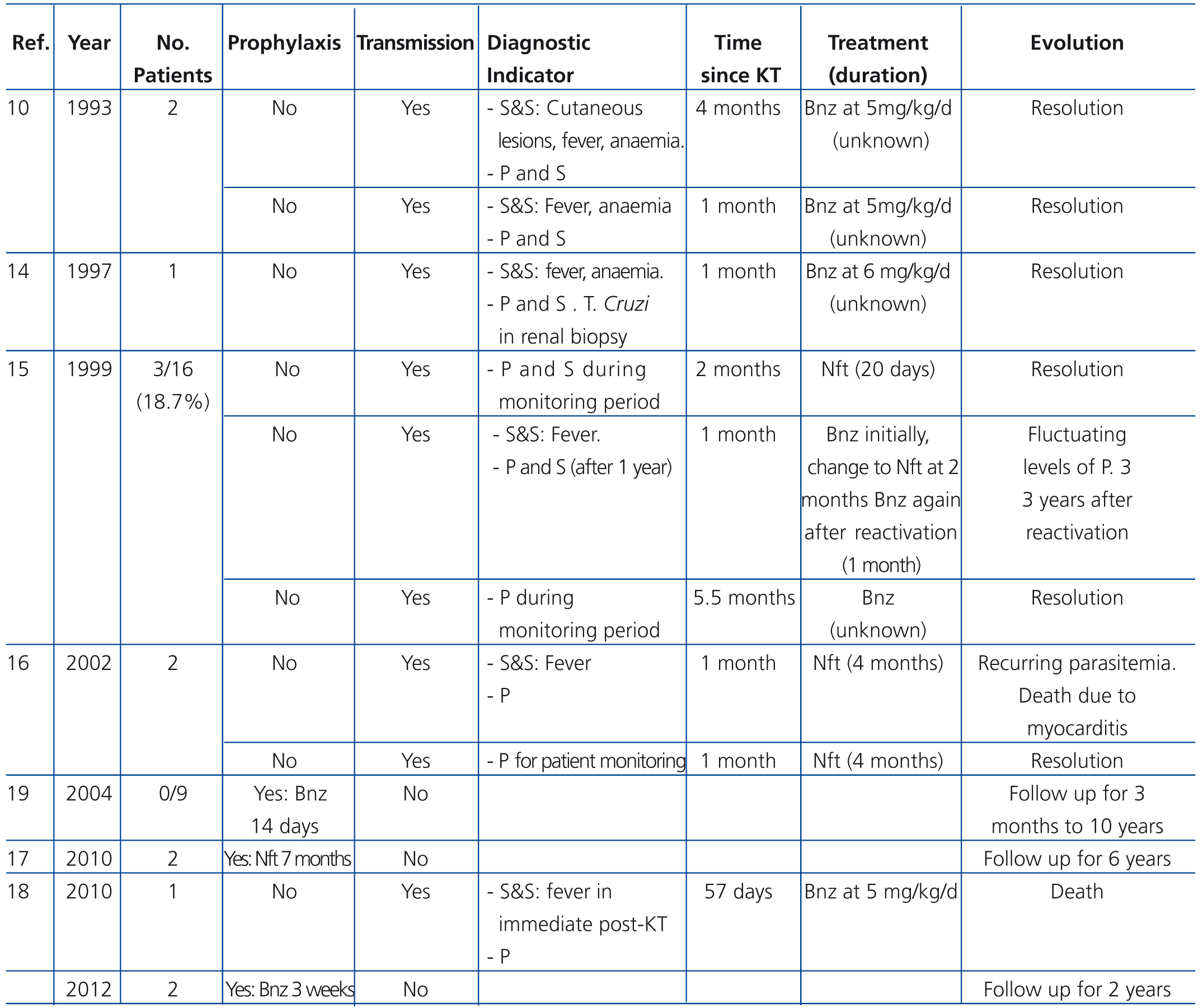
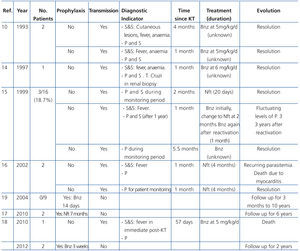
The first medical articles reporting experience in KT and CD were published in the late 1970’s,7 and later publications reported the transmission of CD through kidney grafts,8-13 even the presence of T. cruzi amastigotes in kidney graft biopsies (Table 2). Riarte et al. published a series reporting 16 negative recipients who received kidneys from donors with undetermined CD status. None received prophylaxis in the post-transplant period, and all received conventional immunosuppression therapy. Transmission of the disease was detected in 3 of these cases (18.7%), with disease being diagnosed between 1 and 6 months following KT due to the appearance of parasitemia in two cases and one febrile syndrome detected early. The patients received treatment with benznidazole with varying levels of tolerance but good response in all cases. During the follow-up period (1.5-5 years), only one patient suffered a new reactivation of the disease, which occurred 3 years following KT in the context of treatment for chronic graft rejection.15
The Centre for Disease Control (CDC) in the USA published in 2002 a report of the transmission of T. cruzi in 2 KT recipients from the same donor. One of the recipients developed clinical CD in the form of chagasic cardiomyopathy, and the other displayed only positive serology results.16 Another publication reported a case of KT from a live donor in which no transmission of disease was detected in 6 years of follow-up.17 More recently, a case report was published regarding KT from a cadaveric donor, with late detection of disease transmission following the appearance of febrile syndrome that ended in patient death.18 The largest series recently published involved 9 cases of negative recipients who received kidneys from positive donors. These patients received a prophylactic regimen of benznidazole (5mg/kg/day for 14 days starting at day 0) and conventional immunosuppression. None of the patients presented signs of disease transmission during the follow-up period (3 months – 10 years).19
Currently, the recommendations for monitoring KT recipients from donors with CD consists of parasitological or serological tests (according to the capabilities of each centre) with the following frequency: pre-KT: weekly for the first 2 months, post-KT: every 15 days until 6 months post-KT, and every year thereafter.20 This strict follow-up regimen allows for early detection of disease transmission and the start of specific treatment.
The issue of whether or not to administer primary prophylaxis has been the subject of debate since the very first cases of solid organ transplants were described in donors with CD. In some cases and series published on KT, no prophylaxis has been administered,3,10,15,16,18 whereas others do report prophylaxis, primarily with benznidazole (Table 2).17,19 In cases where prophylaxis was not administered, parasite transmission has been reported in some or all of the patients evaluated in each article. For the most part, these are isolated cases, not case series, which impedes comparison with possible pairs of Chagas-positive donors and a recipient who has yet to show signs of transmission. In the study by Riarte et al., despite the fact that a lack of prophylactic treatment produced transmission of T. cruzi in 18% of cases, this group did not recommend primary prophylaxis, justifying their stance by the absence of cases of severe disease due to early detection and proper response to treatments applied.14 In cases where prophylaxis was applied, no cases of disease transmission have been reported, nor have any complications been observed in relation to treatment.17,19
A working group formed by the Spanish Society for Tropical Medicine and International Health, the Barcelona Research Centre for International Health (CRESIB), and several international experts has recently published a document outlining recommendations for the management of these cases.20 Given the fact that early treatment of these infections is highly effective, there is no clear evidence from specific studies demonstrating a benefit from using prophylaxis, and given the overall experience gained in this field, this group recommends treatment only when there is evidence of disease transmission (positive parasitological or serological test results). As such, there is no clear single criterion for its use. However, given the results from the pertinent literature with an absence of transmission when using prophylaxis, and until more definitive evidence is provided, it would seem advisable to provide prophylaxis in the majority of patients. If prophylaxis is provided, it should be in the form of benznidazole during 1 month at 5mg/kg/day.20
If parasitemia and/or positive serology results arise, treatment must be provided regardless of the associated symptoms.15,20 Two different therapeutic options are available: benznidazole (5mg/kg/24h) and nifurtimox (8mg/kg/24h), both for 60 days’ duration.20 Benznidazole, an active drug against the various forms of T. cruzi, is the first option for treatment given the better tolerance it produces in patients and the absence of an interaction with immunosuppressant drugs. The most common secondary side effects of this drug are the appearance of cutaneous rash associated with photo-sensitivity (30%) and peripheral neuropathy (12%-30%). Although less common, it is also important to control myelotoxicity and the appearance of leuko-thrombocytopenia.5,21 Simultaneous alcohol intake may trigger antabus-like symptoms.5
No randomised clinical studies exist in the medical literature that evaluate the relationship between immunosuppressant treatment in KT and transmission or reactivation of CD. In contrast, a multitude of publications analyse the relationship between this type of treatment and CD reactivation in solid organ transplants in recipients with chagasic cardiomyopathy, and many of the current recommendations have been extrapolated from these studies. The use of anti-thymocyte immunoglobulin in heart transplant cases for chagasic recipients has been shown to increase the rate of CD reactivations, primarily in the context of treatment for episodes of acute rejection. These results have led to recommendations for avoiding the use of this immunosuppression in cases of positive donors and negative recipients, substituting treatment with monoclonal antibodies such as basiliximab.3,22
In a retrospective study, the number of reactivations of CD was significantly lower in patients who received lower doses of cyclosporine (5-10mg/kg vs. 3-5mg/kg).23 One of the most heavily analysed immunosuppressant drugs in relation to CD is mycophenolate mofetil (MMF). A retrospective study of recipients with chagasic cardiomyopathy who received heart transplants compared the incidence of reactivation of CD between patients who received azathioprine as a third immunosuppressant drug (in addition to cyclosporine and prednisone) and those who received MMF. The authors observed a greater incidence and early onset of CD reactivation in patients who received MMF (86.6%) as compared to those who received azathioprine (37.5%) with a 2-year follow-up period. Treatment with MMF was an independent predictor for reactivation.24 Other retrospective studies carried out in patients receiving heart transplants demonstrated a similar relationship.22,25 It does appear that rapamycin inhibits the growth of Trypanosoma bricei,26 which would indicate that mTOR inhibitors could be a good alternative for the use of MMF. Essentially, insufficient evidence exists for recommending specific immunosuppression regimens for these cases, although it is recommended that the use of anti-thymocyte immunoglobulins should be avoided and the use of MMF should be minimised, in addition to maintaining immunosuppression therapies in general at the lowest tolerated doses.3,20
To conclude, CD is an uncommon pathology in our country, but due to current trends in population movements, it is becoming a more and more frequent occurrence, with potential increases in the frequency of kidney donors with a history of CD. The transmission rate of CD in KT recipients is low, and the treatment of patients in cases of transmission is effective. Exhaustive clinical and serological follow-up of these patients is essential in order to ensure early detection of transmissions and start the appropriate treatment regimen, since the evolution of patients in this context is much more favourable. Despite these general recommendations, prospective studies are necessary in order to establish protocols for treatment and monitoring.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
KEY CONCEPTS
1. Screening is necessary involving serological tests for Trypanosoma cruzi in at-risk donors: those who are born in endemic areas (Latin American countries), who have lived for more than one month in these areas, or who have received blood transfusions in these zones.
2. Positive serological test results in a donor, in the absence of clinical symptoms, are not a contraindication for kidney donation.
3. It is recommendable to avoid the use of anti-thymocyte globulins and to minimise immunosuppression.
4. It appears advisable to provide prophylaxis with benznidazole in transplant recipients, although it is necessary to perform an individualised evaluation, taking special care to evaluate basal immunological state and the immunosuppression regimen that will be administered.
5. An exhaustive serological follow-up is necessary to facilitate early detection of transmission.
6. In the case of positive parasitemia and/or serological test results, specific treatment must be instated with benznidazole.
Table 1. Evolution of renal function and immunosuppression therapy after 1 and 2 years in two recipients of kidneys from a donor with positive serology for Trypanosoma cruzi
Table 2. Experience published in the medical literature in the last two decades regarding kidney donors with Chagas disease