A child's visit to a healthcare facility is often a situation of psychosocial stress associated with fear and anxiety. This situation can generate a transient cardiovascular response with an increase in the initial blood pressure (BP) measurements, what is known as the "white coat phenomenon".1 Although this response is generally short-lived,2 repetitive stimulation of the cardiovascular system can lead to a sustained increase in BP.3
Natural disasters are acute, high-intensity stressors. The hypertensive reaction they produce in adults has been characterized during earthquakes,4,5 with a return to normal that can take up to 14 months.6
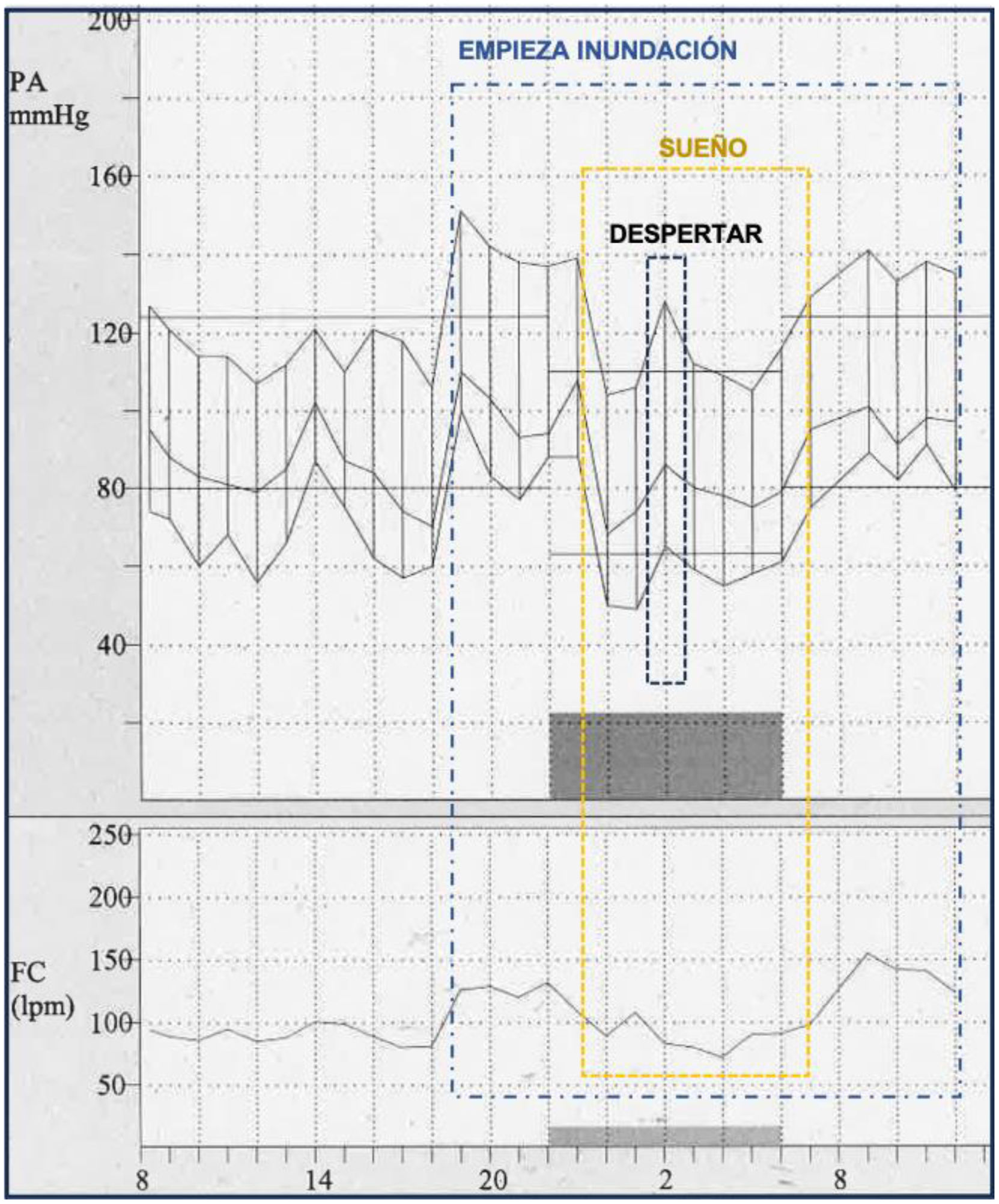
We present the hypertensive response in an 11-year-old girl during the flooding caused by storm DANA that affected the towns of southern Valencia in October 2024. The blood pressure was recorded by ambulatory blood pressure monitoring (ABPM) at home for 36 h. The patient was followed in our department for renovascular arterial hypertension (HTN) controlled with moderate doses of enalapril and undergoing follow-up ABPM. Blood pressure was recorded using a Spacelabs 90217A oscillometric device, which was started in the hospital at 8:20 a.m. on Tuesday, October 29, and programmed to measure at 20-min intervals during wakefulness (8 a.m. to 9 p.m.) and every 30 min during sleep (10 p.m. to 7 a.m.).
The patient lived in the town of Albal (Valencia), where the flooding began around 6:50 PM. The ABPM functioned adequately throughout the duration of the disaster, with a 95% valid reading percentage. The ABPM was removed at home at 12 PM the following day.
As shown in Fig. 1, systolic blood pressure, diastolic blood pressure (SBP/DBP), and heart rate (HR) were within normal ranges, 106/60 mmHg and 80 bpm, respectively, one hour before the onset of the event. An increase in these parameters was observed from 7 PM and for the following 5 h. Mean arterial pressure (MAP) increases by a maximum of 57% during the first hour of the catastrophe, rising by 42% in the following 4 h, with a 52% increase in HR during this time. The maximum SBP/DBP is 151/100 mmHg and the minimum 138/77 mmHg. At 11:30 pm, when the patient falls asleep, BP drops to normal levels. A significant increase is observed upon awakening, which normalizes upon falling asleep again. Finally, at 9 am the following day (upon awakening), BP and HR levels return to hypertension values similar to those at the beginning of the catastrophe (SBP/DBP 135/79 mmHg [27/31% increase]); HR 124 bpm (53% increase). The vasopressor effect persisted 18 h after the onset of the catastrophe when the device was turned off at 12:30 p.m. ABPM was repeated 3 weeks later, and BP and HR values had normalized.
This publication is the first direct, live evidence of the cardiovascular effect of a natural disaster, such as a flood, in a pediatric patient.
The flood caused a sharp increase in BP and HR in our patient, which persisted for 18 h after its onset, normalizing during sleep and extinguishing on follow-up ABPM 3 weeks later. This chronology of response to the stressor demonstrates both a cardiac and vascular response in the acute phase, presumably associated with an activation of the sympathetic nervous system, which appears to be responsible for the increased rate of acute myocardial infarction and sudden death described in this type of disaster.7 The intense variability in BP maintained over time (if the stressor persists) may be related to morbidity and mortality in adults.8 A return to normal, if the stressor ends, has also been described in adults.4–6
The usefulness of ABPM in diagnosing masked hypertension related to stressors that go undetected in the clinical interview is particularly important in the pediatric population, where expressing distress, nervousness, and anxiety is difficult. This can help us detect alternative diagnoses to organic pathology, including situations of abuse/mistreatment within the family or at school.
In conclusion, acute and chronic stressful situations, such as the one recently experienced in the Valencia region, have a health impact that often goes unnoticed in the pediatric population. This study demonstrates the severe anxiety experienced by the patient in the hours following the event and the resulting cardiovascular impact.