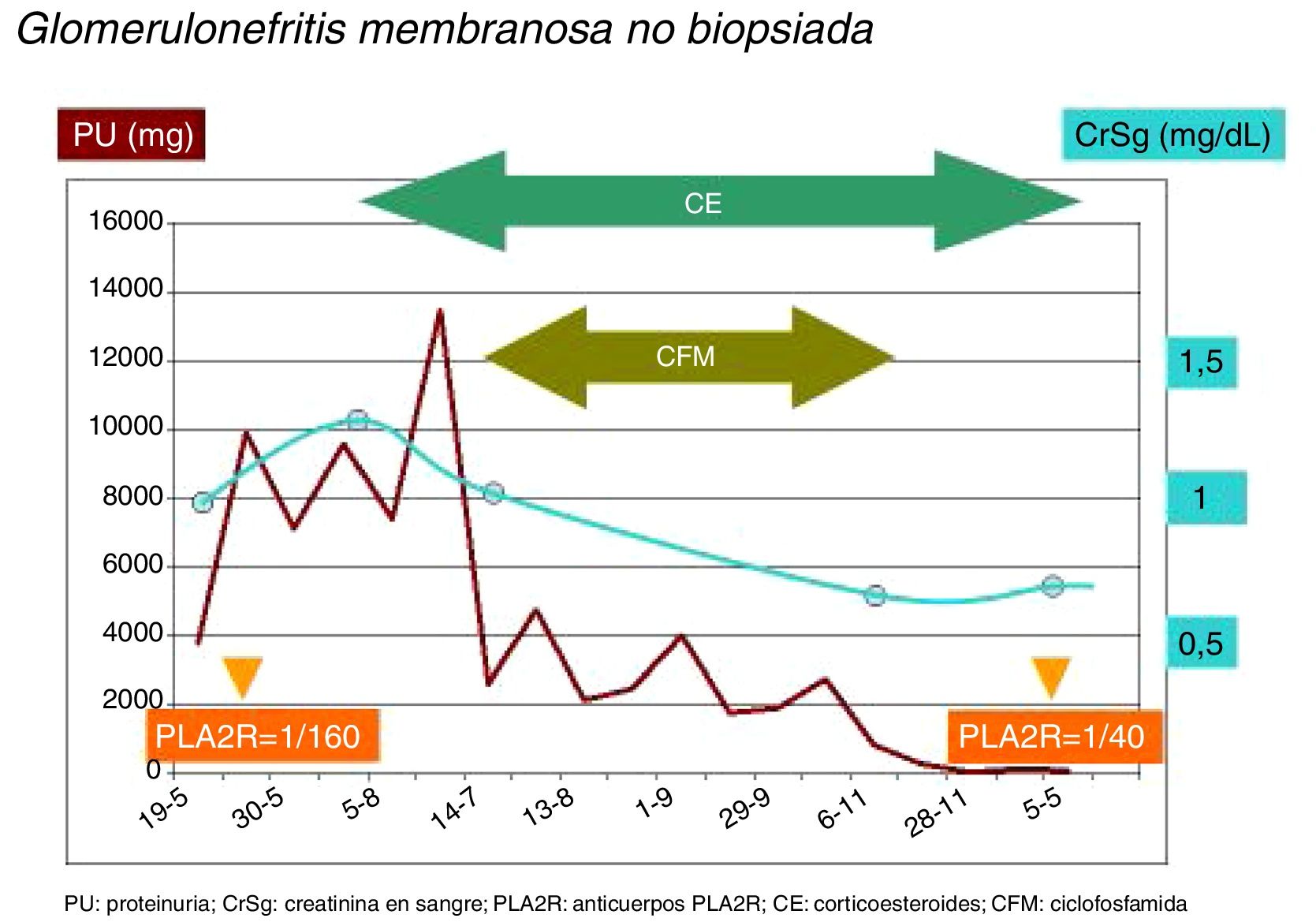
We present the case of a 71-year-old man, hypertensive, with a 3 weeks history of edema on the eyelids and lower limbs. The following data were observed: Hematology: leukocytes: 11,700×103μm−1; hemoglobin: 12.2g/dl, and platelets: 36,900×103μm−1. Biochemical profile: creatinine: 1.2mg/dl; glomerular filtration rate (CKD-EPI): 60.2ml/min; cholesterol: 325mg/dl; HDL: 56mg/dl; LDL: 238mg/dl, and calcium: 10.2mq/dl. In 24h urine: proteinuria: 13,530mg with microhematuria. Immunology w/u without hypocomplementemia, mild decrease in immunoglobulin G. Rheumatoid factor, anti-nuclear antibodies, anti-neutrophil cytoplasm antibodies, anti-glomerular basement membrane antibodies were negative and there were positive only the anti-PLA2r antibodies 1/160. In the ultrasound study: normal kidneys without vascular or parenchymal damage, ruling out obstruction. The study of possible secondary causes with serologies of hepatitis B, C and HIV negative viruses, chest X-ray and abdominal ultrasound without data suggestive of neoplasia, echocardiogram without data of endocarditis and Bence-Jones proteinuria negative was completed. It was decided to perform a renal biopsy, but the previous day began with dry cough, dyspnea and desaturation (90%), so a lung scan was performed in which pulmonary thromboembolism was observed, anticoagulation was started and no renal biopsy could be performed. With these data and given the positivity of M-type phospholipase A2 receptor antibodies (anti-PLA2R), a diagnosis of possible membranous nephropathy was made and empirical treatment was decided with corticosteroids and oral cyclophosphamide with favorable response of the nephrotic syndrome and complete remission (Fig. 1).
Primary membranous nephropathy, a frequent cause of nephrotic syndrome, is an antibody-mediated glomerular disease. Since 2009, in which Beck discovered the antigen involved, PLA2R, there have been multiple advances on the of diagnostic value and predictive power of PLA2R.1,2 Anti-PLA2R antibodies are present in 70–80% of primary membranous nephropathies (in podocytes, formed in situ together with IgG),1,3 in a 5–10% of cases there is another antibody involved, thrombospondin (THSD7A), and in the rest of patients the causal antibody remains to be identified.4
The presence of anti-PLA2R antibodies has a sensitivity higher than 70%, and a specificity of almost 100% for the diagnosis of membranous nephropathy.4–6 The severity of the disease is associated to higher level of AB, with greater proteinuria and less possibility of spontaneous remission.2,7–10 In addition, the level of anti-PLA2R antibodies may serve as a biological marker, since the immune response precedes the appearance of proteinuria and the reduction of antibodies is often seen before the resolution of proteinuria.1,2,4,6,8–10 Thus, the presence of anti-PLA2R antibodies in serum has been considered a signal of active disease suggesting early immunosuppressive treatment without the need to complete the 6 months of support treatment.4–10 The high specificity of these antibodies has already posed the possibility of assuming an accurate diagnosis and especially in those cases, such as ours, in which there is a very high or unacceptable risk of performing a renal biopsy.4,6,7
Finally, in terms of treatment, good results have always been obtained with the combination of corticosteroids and cyclophosphamide.
Please cite this article as: Ruiz Martínez L, Fernández Fresnedo G, Rodrigo E, Heras M. ¿Podemos prescindir de la biopsia renal en la nefropatía membranosa en caso de anticuerpos anti-PLA2R positivos? Nefrologia. 2019;39:311–312.