Tertiary hyperparathyroidism (THPT) occurs in 2–25% of renal transplant patients with normal renal function. THPT is due to the autonomous proliferation of the parathyroid glands.1,2 Hypercalcemia impairs renal function through vasoconstriction and causes tubulointerstitial calcifications, which limits long-term graft survival.3 Therefore, early treatment of hypercalcemia is important to prevent deterioration of renal graft function.
Until year 2005, when calcimimetics became available, surgical treatment of THPT was the only effective strategy to control hypercalcemia in renal transplant patients.3,4 The calcimimetic, cinacalcet controls hypercalcemia without affecting renal function.5,6 However, while cinacalcet reduces the need for parathyroidectomy in patients with severe secondary hyperparathyroidism,7 in the tertiary this beneficial effect has not been confirmed.5,6
The objective of the study is to analyze the impact that cinacalcet has had on parathyroidectomies for the treatment THPT in our center after 10 years of use.
The study included renal transplant patients with normal renal function who required parathyroidectomy between January 1995 and December 2014. Cases with prior thyroid and/or parathyroid surgery and those with syndrome of MEN were excluded. For the analysis of the data, two periods are differentiated separated by the introduction of cinacalcet in our center: (1) pre-cinacalcet period: 1995–2004; and (2) post-cinacalcet period: 2005–2014. In THPT surgery was performed in cases with hypercalcemia that did not respond to conservative measures. Both groups differ in the use of cinacalcet prior to surgery. Epidemiological, clinical, therapeutic and follow-up variables are analyzed. For statistical analysis, the SPSS 15.0® software for Windows® is used, using the chi-squared test, the Fisher exact test, the Student's t-test and the Mann–Whitney U test.
Selection criteria were fulfilled by 24 kidney transplant recipients, with a mean age of 47.9±8.2 years, 66.7% (n=16) were male. Twenty three patients (95.8%) were on hemodialysis and one (4.2%) was on peritoneal dialysis, with a mean time of 6.6±5.3 years prior to receiving the last transplant. 33.3% (n=8) received more than one kidney transplant. The mean time from renal transplantation to parathyroidectomy was 37±32.3 months (3–115 months).
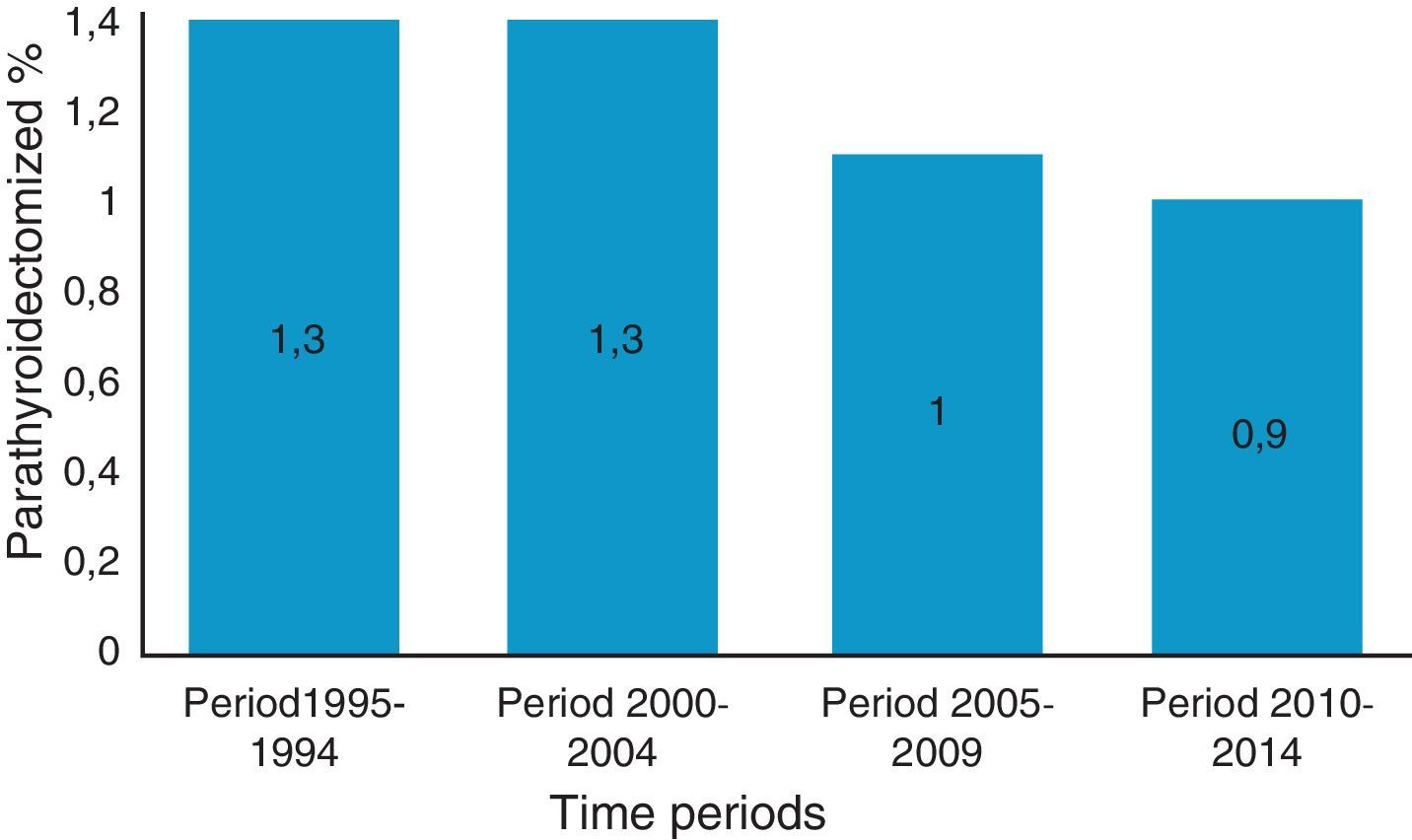
Fifty-four percent of patients (n=13) were parathyroidectomized during the pre-cinacalcet period and the remaining 46% (n=11) during post-cinacalcet (p>0.05). Regarding the total number of kidney transplant patients with acceptable renal function per year, parathyroidectomy was performed in 1.3% of patients per year during pre-cinacalcet period as compared with a 1% in the post-cinacalcet period (p>0.05) (Fig. 1).
Comparison of patients from the pre and post cinacalcet era shows that there were no differences in the variables analyzed, except for Two. First all patients (n=13) receiving parathyroidectomy during the post-cinacalcet period were asymptomatic compared to n=7 patients (34%) in the pre-cincalcet period (p=0.016). Most symptomatic patients had pain in bone and joints. The second difference was the serum phosphorus concentration, which was lower in the post-cinacalcet than pre-cinacalcet group (2.3±0.2mg/dl versus 2.8±0.4mg/dl; p=0.011). In all cases, the surgical treatment was subtotal parathyroidectomy. There was a reoccurrence of HPT in 4.2% in the pre-cinacalcet group, which is now controlled with cinacalcet t.
As opposed to what is being described regarding secondary hyperparathyroidism, with approval of cinacalcet by the European Medication Agency, there has been no decrease in the number of indications for parathyroidectomy in THPT. However, we have observed that patients on cinacalcet are asymptomatic at the time of surgery. Thus both treatments improve patient's quality of life.
If surgery is required, subtotal parathyroidectomy shows very acceptable results with low recurrence rates if performed in endocrine surgical units with experience.8
In conclusion, cinacalcet has not been able to reduce the surgical indications of THPT, although patients with surgical indication have fewer symptoms.
Please cite this article as: Ruiz J, Ríos A, Rodríguez JM, Llorente S, Jimeno L, Parrilla P. Los calcimiméticos no han tenido impacto en la cirugía del hiperparatiroidismo terciario. Nefrologia. 2017;37:651–653.