Dear Editor,
Hypercalcaemic crisis is a rare form of presentation of primary hyperparathyroidism. Only small case series have been reported in the literature1,2. It is characterised by severe hypercalcaemia, renal failure and an altered state of consciousness. We present the case of a 70-year-old patient, who was admitted for acute kidney injury caused by a hypercalcaemic crisis within the context of previously undetected primary hyperparathyroidism. The therapeutic approach and patient progress are discussed.
Clinical CaseThe patient is a 70-year-old white male with a history of benign prostatic hyperplasia, recurrent atrial fibrillation and right hemithyroidectomy due to nodular hyperplasia, as well as chronic kidney disease that had not been studied (baseline creatinine 1.5 mg/dL).
He was admitted to the emergency room due to symptoms that included unsteady gait and generalized weakness, which had been progressing in the last three months and for which the patient had been previously treated at another hospital. Upon physical examination, the patient was dehydrated, conf used, brady psychic, and presented distal tremor.
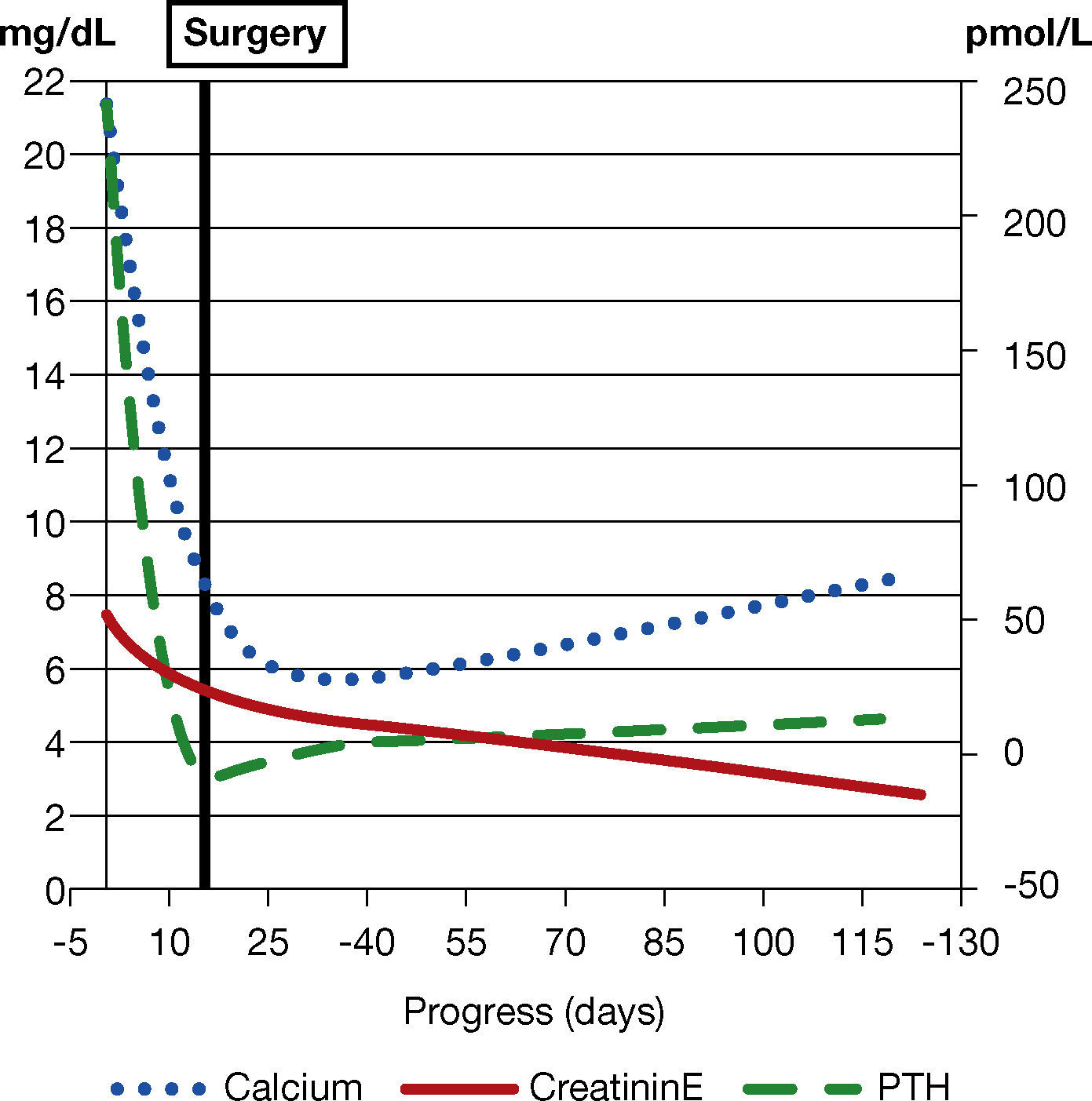
Table 1 summarizes the laboratory data, which highlight a significant deterioration in renal function, severe hypercalcaemia and marked increase in PTH levels (20 times the laboratory reference value). Treatment was initiated with IV fluid therapy, infusion of furosemide, and intravenous corticosteroids, bisphosphonates and calcitonin. Due to the severity of the neurological symptoms, urgent simultaneous renal replacement therapy was indicated by means of haemodialysis with low calcium dialysate. The patient showed temporary clinical improvement, but, due to the persistent renal failure and rebound hypercalcaemia (increase in blood calcium level > 2 mg/dL 24hours post-haemodialysis), continued daily session were required.
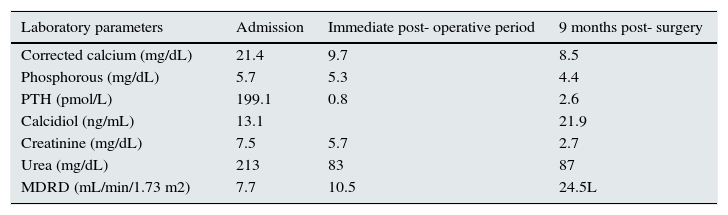
– Baseline and progressive laboratory data.
| Laboratory parameters | Admission | Immediate post- operative period | 9 months post- surgery |
|---|---|---|---|
| Corrected calcium (mg/dL) | 21.4 | 9.7 | 8.5 |
| Phosphorous (mg/dL) | 5.7 | 5.3 | 4.4 |
| PTH (pmol/L) | 199.1 | 0.8 | 2.6 |
| Calcidiol (ng/mL) | 13.1 | 21.9 | |
| Creatinine (mg/dL) | 7.5 | 5.7 | 2.7 |
| Urea (mg/dL) | 213 | 83 | 87 |
| MDRD (mL/min/1.73 m2) | 7.7 | 10.5 | 24.5L |
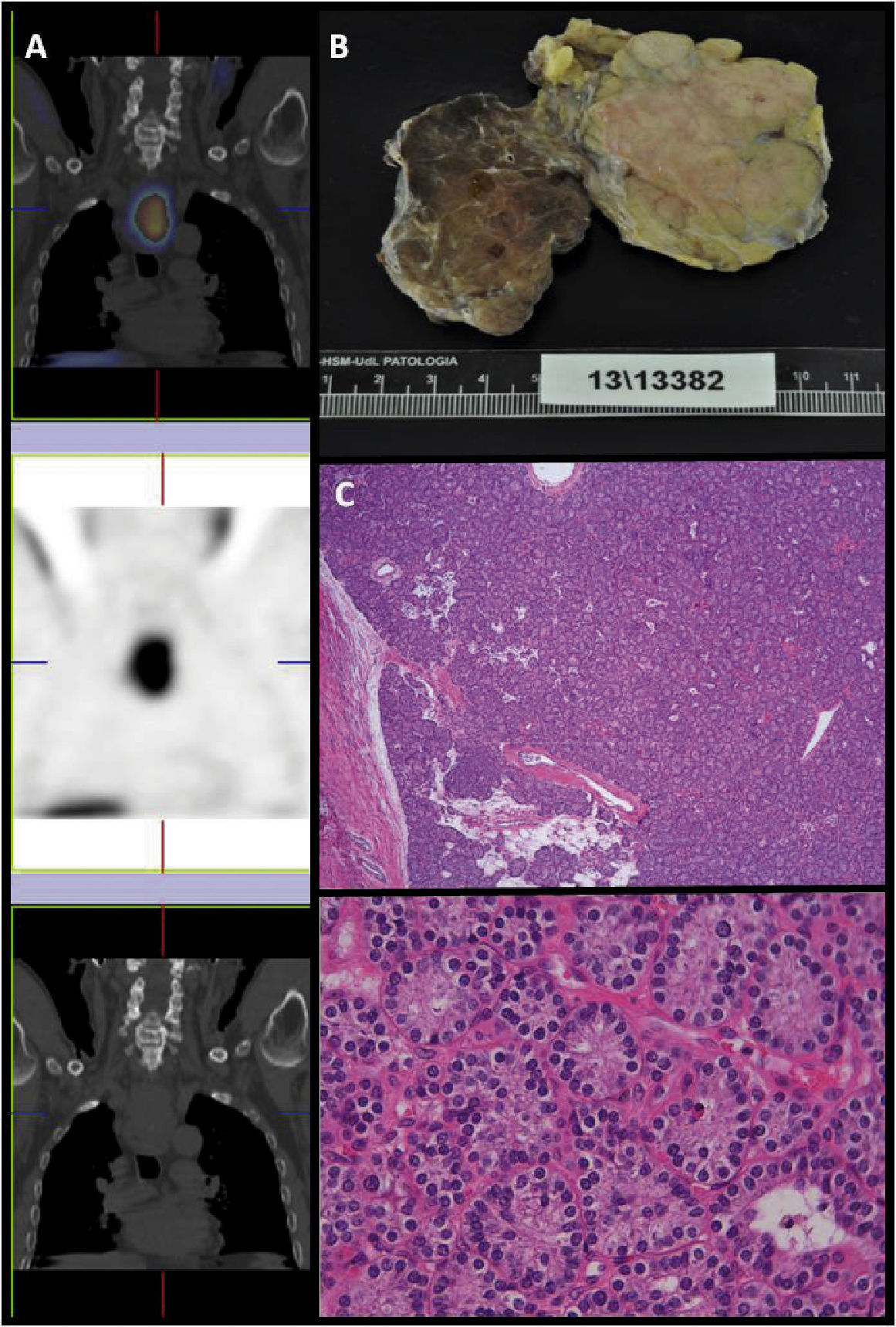
The etiologic study ruled out myeloproliferative processes and other neoplasms (no monoclonal component in the protein analysis; negative Bence-Jones proteinuria), infectious disease (nonreactive serology) and autoimmune diseases. Renal ultrasound demonstrated normal-sized kidneys and good cortico-medullary differentiation. The thoracic-abdominal CT scan showed a retroesophageal mass measuring 5.6 × 3.2 × 6.8cm, which was suspicious for parathyroid tumour, in addition to bilateral hypodense adrenal nodules: right 27 × 18mm and left 15 × 11mm. Parathyroid scintigraphy confirmed the image (Figure 1A).
The Endocrinology Unit was consulted about these findings, and phaeochromocytoma was ruled out (negative urine catecholamine and metanephrine). In a joint session with the General Surgery Unit, surgical management was decided upon, which included resection of an 8-cm parathyroid tumour (Figure 1B). The Pathology Unit reported the mass to be a parathyroid adenoma with no capsular or vascular invasion (Figure 1C).
During the immediate post-operative period, the patient developed “hungry bone syndrome” and therefore required intravenous and oral calcium supplementation for severe hypocalcaemia as well as daily haemodialysis sessions until nine days after the surgery.
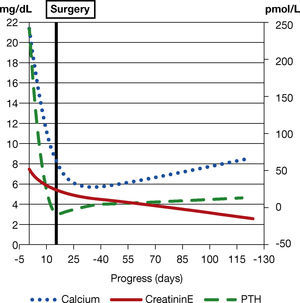
Nine months later, the patient is asymptomatic, with calcaemia within normal limits and no need for supplements as well as partial recovery of renal function (creatinine 2.7 mg/ dL, Figure 2). It should be noted that renal function is still altered one year after the surgery, despite calcaemia normalization.
The great majority of parathyroid adenomas are asymptomatic, and only a small percentage cause severe hypercalcaemia and renal failure requiring renal replacement therapy3,4. A recent and extensive literature review only identified 17 cases of hypercalcaemia > 20 mg/dL, with a mortality rate of 60%5. There are only three cases reported with calcaemia > 30 mg/dL6–8.
The most relevant aspects in this case report are:
- •
The onset of a parathyroid adenoma as severe hypercalcaemia
- •
Renal failure secondary to hypercalcaemia crisis that required renal replacement therapy and only partially recovered after correcting the cause of the hypercalcaemia
- •
The large size of the parathyroid tumour with non-malignant histology