Percutaneous pharmacomechanical thrombectomy is a useful treatment in the management of arterial and deep vein thrombosis, as well as in thrombosed vascular grafts for haemodialysis.1 The AngioJet® system fragments and extracts the thrombus combining pharmacological thrombolysis through infusion of a thrombolytic agent instead of occlusion with mechanical thrombectomy using hydrodynamic technology. The catheter applies a high-pressure jet of saline solution which creates a localised area of low pressure at the tip, generating a Venturi (vacuum) effect which enables thrombus fragmentation and aspiration. In the field of Nephrology, it is one of the possible therapeutic indications in vascular access thrombosis. In general, this technique is well tolerated, with a low rate of complications. The most common are vessel dissection and perforation, distal embolisation, cardiac arrhythmias, haemolysis with subsequent myoglobinuria and acute renal failure.2,3 Some cases of pancreatitis have also been reported.3
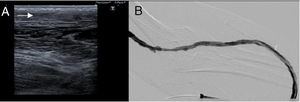
We present the case of a 79-year-old male with chronic kidney disease (CKD) secondary to nephroangiosclerosis and diabetic nephropathy who has been on a haemodialysis programme since 2016. A loop-type left forearm humerocephalic prosthesis was used as vascular access, performed in July 2016. Subsequently, he had two episodes of juxta-anastomotic venous stenoses resolved using balloon angioplasty, and in June 2017 he presented complete thrombosis treated with thrombolysis using AngioJet®, with no complications. In August 2017, he attended dialysis with thrombosis of the graft documented by Doppler ultrasonography (Fig. 1). Thrombectomy was performed using AngioJet®, which was carried out with no immediate complications and with a good morphological and haemodynamic result (Fig. 1B). Then, 1h later, 60min of dialysis was scheduled through prosthetic repair, which took place without incidents. Thirty minutes after finishing the session, the patient reported nausea, numbness of the tongue and dyspnoea. Methylprednisolone was administered, with no improvement in the symptoms. Subsequently, he presented with a fever (38.5°C), hypertensive crisis (240/120mmHg) and oxygen desaturation of down to 65%. Hyperlactacidaemia and neutrophilic leukocytosis were observed in the initial analysis. He was therefore monitored and empirical antibiotic therapy with vancomycin and meropenem was started. Twelve hours later, the patient was asymptomatic and stable, jaundice was observed and lab tests revealed hyperbilirubinaemia, hypertransaminasaemia and increased pancreatic amylase and lipase, together with increased lactate dehydrogenase and decreased haptoglobin (Table 1). In view of these findings, the patient was diagnosed of acute haemolysis secondary to AngioJet® thrombectomy with hepatopancreatic involvement. Since the patient had no other predisposing factors (such as history of biliary lithiasis, previous pancreatitis or alcohol consumption), it was analysed in the context of a pancreatic reaction secondary to haemolysis. The patient remained afebrile with bowel resting for three days, with signs of gradual improvement, and was discharged six days after the onset of symptoms.
Progression of analytical parameters after the procedure.
| Time after thrombectomy | 2h | 1 day | 2 days | 5 days | 8 days | 12 days |
|---|---|---|---|---|---|---|
| Haemoglobin (g/dl) | 10.5 | 11.6 | 10.2 | 8.8 | 8.9 | 8.9 |
| LDH (IU/l) | 3109 | 992 | 439 | 288 | 219 | |
| Haptoglobin (mg/dl) | 103 | <6.5 | 135 | 147 | ||
| Amylase (IU/l) | 1625 | 1493 | 140 | 203 | 186 | |
| Lipase (IU/l) | 47 | 137 | 87 | |||
| AST (IU/l) | 1576 | 347 | 32 | 19 | 12 | |
| ALT (IU/l) | 1095 | 633 | 131 | 36 | 19 | |
| Total bilirubin (mg/dl) | 1.3 | 7.4 | 1.7 | 0.7 | 0.4 | 0.4 |
| Indirect bilirubin (mg/dl) | 1.2 | 2.0 | 0.3 | |||
| Direct bilirubin (mg/dl) | 0.1 | 6.4 | 1.4 |
ALT: alanine aminotransferase; AST: aspartate aminotransferase; LDH: lactate dehydrogenase.
Reference ranges: haemoglobin, 13.0–18.0; LDH, 135–225; haptoglobin, 30–200; amylase, 25–100; lipase, 0–60; AST, 0–40; ALT, 0–41; total bilirubin, 0.0–1.2; indirect bilirubin, 0.0–0.9; direct bilirubin, 0.0–0.4.
Intravascular haemolysis after pharmacomechanical thrombectomy has been attributed to entrapment and selective destruction of the thrombus by hydraulic recirculation through a high-speed retrograde current produced by the high-pressure output of saline. This current of fluid generates a pressure gradient that traps, dissolves and evacuates the thrombus by aspiration, causing red blood cell trauma and subsequent haemolysis. Pancreatitis secondary to haemolysis of various causes is well known, although its physiopathology is not so well understood.4 There is evidence from animal models that a released heme group may promote the activation of neutrophils (with proteolytic and oxidative potential), regulates the activation of alpha-2-macroglobulin (as an acute-phase reactant) and promotes the intravascular coagulation and generation of oxygen-free radicals in the microvasculature of the pancreas. All of these are mechanisms proposed for the pancreatic lesion.5 The risk of haemolysis is probably related to several factors, including the size of the thrombus, the blood flow within the vessel and the duration of the procedure. In the literature, there are 10 cases of pancreatitis after AngioJet® thrombectomy,2,6–9 and only one case of trombectomy of a vascular prosthesis for haemodialysis.8 Symptoms may develop during the first 24h or even after 4 days of the procedure. Progression was favourable in all cases and most of them only received conservative treatment. In our case, in addition to the pancreatic reaction, we observed acute hepatitis associated with intravascular haemolysis, which could be explained by the same pathophysiological mechanism. This is therefore the first case in the literature of hepatitis associated with haemolysis due to thrombectomy.
Percutaneous pharmacomechanical thrombectomy using AngioJet® is a useful procedure to rescue thrombosed vascular access grafts, increasing their survival. However, it is not a risk-free technique. Although haemolytic pancreatitis is a rare adverse effect, it may be severe so the nephrologist must be alert about this possible complication.
Please cite this article as: Urdaneta J, Arroyo D, Mon C, Abadal J, Gálvez E, Ortiz M, et al. Pancreatitis y hepatitis agudas por hemólisis secundaria a trombectomía farmacomecánica percutánea de acceso vascular protésico para hemodiálisis. Nefrologia. 2019;39:104–105.