Chronic kidney disease (CKD) poses a significant public health challenge worldwide and its prevalence is rising due to aging populations and increasing risk factors. The CARABELA-CKD initiative aims to address CKD management inefficiencies.
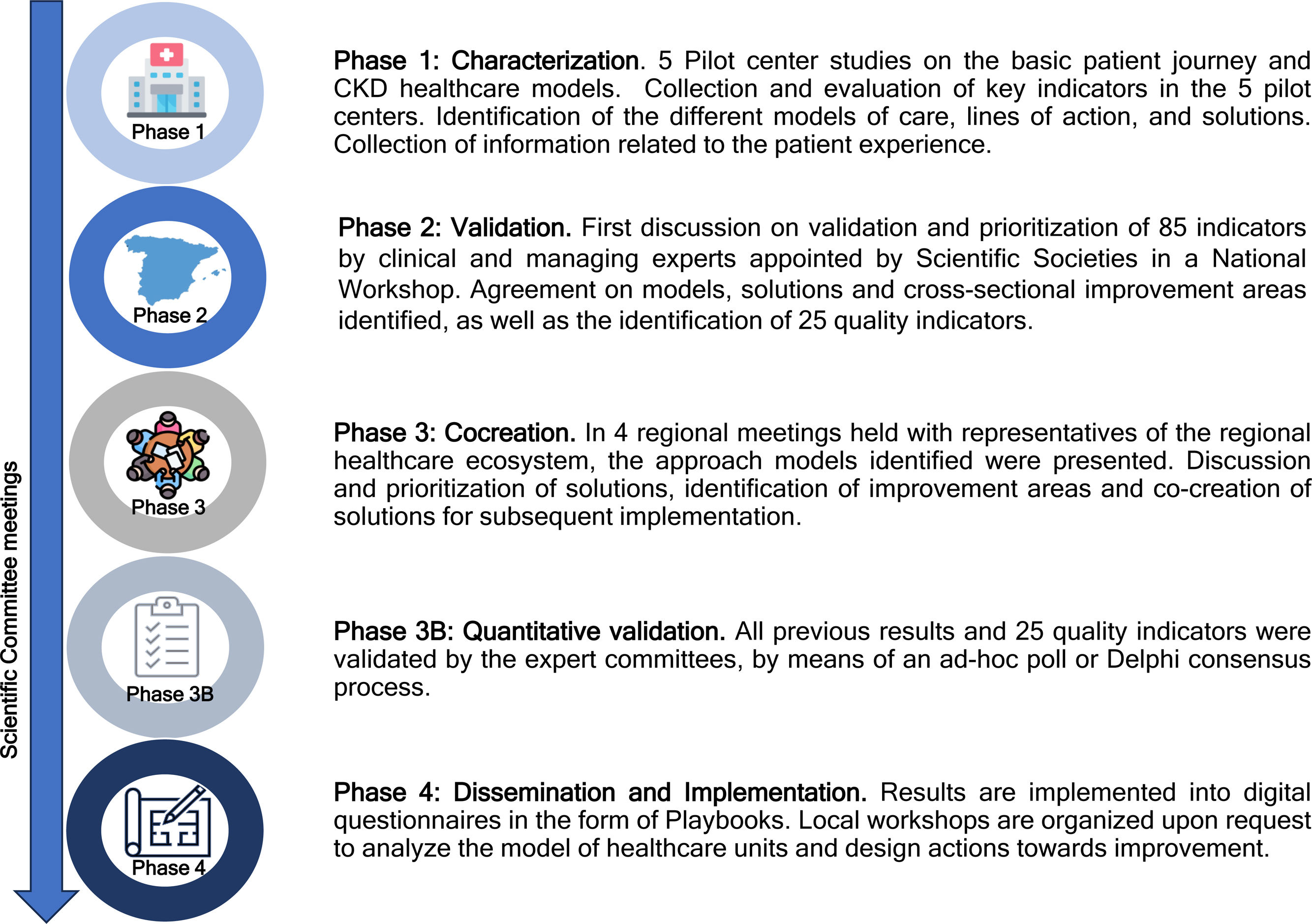
Materials and methodsThe CARABELA-CKD initiative was structured into four phases. The methodology involved five pilot center studies, conducted to characterize CKD healthcare models (Phase 1), followed by the validation of disease care models, improvement areas, potential solutions, and strategic healthcare quality indicators in a National Multidisciplinary Workshop (Phase 2). Regional meetings were then held to refine all these aspects from a regional perspective and to determine the cocreation of solutions with subsequent quantitative validation of results using the two-round Delphi method (Phase 3B). Dissemination and implementation included integrating findings into digital questionnaires creating digital Playbooks and organizing local workshops (Phase 4).
ResultsThe study identified three CKD care models in Spanish hospitals, each with distinct levels of specialization and resource availability. Twenty-five healthcare quality indicators were validated in a national meeting to assess various aspects of care quality and transformation. Improvement areas were identified, leading to the formulation of solutions to enhance CKD care models in Spain.
ConclusionsThe CARABELA-CKD initiative, a collaborative effort between Scientific Societies involved in the CKD care process and AstraZeneca, is a nationwide attempt in Spain to create a framework to promote solutions in healthcare delivery and improvements in the quality of care that result in better health outcomes and higher standards of care quality, improved quality of life for patients, and increased efficiency of the Healthcare Service.
La enfermedad renal crónica (ERC) representa un desafío significativo para la salud pública a nivel mundial. Su prevalencia está en aumento debido al envejecimiento poblacional y a factores de riesgo crecientes. La iniciativa CARABELA-CKD busca abordar las ineficiencias en el manejo de la ERC.
Materiales y métodosLa iniciativa CARABELA-CKD se estructuró en 4 fases. En la primera fase, se caracterizaron los modelos de atención de la ERC en 5 centros piloto. En una segunda fase en una reunión nacional se validaron estos modelos, las áreas de mejora y las soluciones potenciales, además de indicadores de calidad en el manejo de la ERC. En la tercera fase se procedió a realizar reuniones regionales que facilitaron el refinamiento de las soluciones bajo una perspectiva regional con validación cuantitativa de resultados mediante un proceso Delphi (Fase 3B). En la cuarta fase se integraron los hallazgos en cuestionarios digitales permitiendo, mediante talleres, la diseminación e implementación local de CARABELA-CKD.
ResultadosEl estudio identificó 3 modelos de atención de la ERC en hospitales españoles, cada uno con niveles distintos de especialización y disponibilidad de recursos. Se validaron 25 indicadores para evaluar varios aspectos de la calidad de atención y transformación. Se identificaron áreas de mejora, lo que llevó a la formulación de soluciones para mejorar los modelos de atención de la ERC en España.
ConclusionesLa iniciativa CARABELA, entre las sociedades científicas relacionadas con el manejo de la ERC y AstraZeneca, es una iniciativa multidisciplinar a nivel nacional de crear un marco para promover cambios en la atención sanitaria, que resulten en mejoras en los resultados en salud y en estándares más altos de calidad asistencial, mejora en calidad de vida de los pacientes y eficiencia del sistema sanitario.
Chronic kidney disease (CKD) is a public health problem worldwide and is considered a silent epidemic due to the low rate of diagnosis and the lack of awareness of this condition among the population.1–6 Approximately 15% of the Spanish population is affected by CKD.4 The progressive aging of Western society, coupled with the increasing prevalence of arterial hypertension, diabetes mellitus, obesity and heart failure are crucial factors that are driving the progressive rise in the prevalence of CKD.1,7 This results in a heightened risk of premature mortality, especially from cardiovascular causes. If the current trend continues, by 2040, CKD will be the fifth leading cause of death in Spain and by the end of the century, it may possibly rank as the second leading cause of death in Spain.6 Furthermore, there has been a 30% overall rise in advanced CKD necessitating kidney replacement therapies in recent decades in Spain, impacting over 64,000 individuals. The economic burden is substantial, accounting for 3% of total healthcare costs.8 Therefore, developing and implementing strategies aimed at optimizing the management of CKD is absolutely necessary.
The CARABELA-CKD is a strategic initiative developed within the CARABELA framework, designed to tackle the intricate improvement areas associated with CKD management within the Spanish Healthcare Service.9 CARABELA initiatives aim to achieve a thorough understanding of the improvement areas that all stakeholders involved in the care of chronic diseases in the Healthcare Service must address in order to catalyze the transformation in clinical practice needed to achieve improvements in the quality of care. CARABELA initiatives are rooted in lean process reengineering and constitute holistic efforts in which Scientific Societies and AstraZeneca collaborate to examine current improvement areas in chronic diseases. In sum, CARABELA-CKD, spearheaded by a multidisciplinary committee, with the participation of 3 Scientific Societies, represents a comprehensive and transversal initiative aimed at addressing management inequalities and identifying inefficiencies in CKD management in Spain.
This article presents the outcomes of the CARABELA-CKD initiative which focus on assessing the existing CKD management models in Spain to identify improvement areas, solutions and healthcare quality indicators to delineate the action plans.
Materials and methodsDesign and participants of CARABELA-CKDThe overall structure and basis of the CARABELA methodology have been documented previously.9 Specifically, CARABELA-CKD comprised four phases (Fig. 1). Coordination throughout Spain was carried out by the Scientific Societies involved in the care of patients with CKD, namely S.E.N. (Spanish Society of Nephrology), SEEN (Spanish Society of Endocrinology and Nutrition), and SECA (Spanish Society for Healthcare Quality), and AstraZeneca.
Characterization of CKD healthcare models in Spanish hospitals (Phase 1)The characterization phase was framed on the understanding that CKD care is a circular and multidisciplinary process.10 To start, a general model or patient pathway for CKD clinical management was developed by the Scientific Committee and tested in five pilot centers representing the Spanish geography and organizational models, in order to identify variations and adaptations to different settings (Fig. 1). This process led to the categorization of various models of patient care. To evaluate each of the identified models and serve as reference for future monitoring, improvement areas, solutions and a list of healthcare quality indicators were developed by the Scientific Committee for CARABELA-CKD. Results from the first phase were validated by the Scientific Committee in preparation for the National Conference.
Validation of results (Phase 2) and regional (Phase 3) and local (Phase 4) phasesA National Multidisciplinary Workshop was held with 100 representatives from the CKD healthcare ecosystem in Spain. In this meeting, the following actions were implemented: validation of the nine variables that would define and characterize each care model, selection of the strategic healthcare quality indicators using a two-round Delphi survey, and validation of improvement areas and potential solutions applicable to the different CKD healthcare models.
The results of the National Multidisciplinary Workshop were further shared and discussed in a set of four Regional Multidisciplinary Meetings with the participation of physicians representative of the whole Spanish territory, in which local and regional realities were further considered, providing additional insight and opportunities to propose regionally refined solutions and adaptations for various settings. Based on the findings and discussions from the National Multidisciplinary Workshop and the Regional Multidisciplinary Meetings within the CARABELA-CKD initiative, solutions were formulated to address improvement areas within the CKD care process. At present, CARABELA-CKD results serve as the basis for an ongoing practical phase, in which improvement areas and solutions are implemented into digital questionnaires in the form of Playbooks. Local workshops to analyze the model of healthcare units and design tailored actions toward improvement in the care of CKD are organized in healthcare areas throughout Spain upon request.
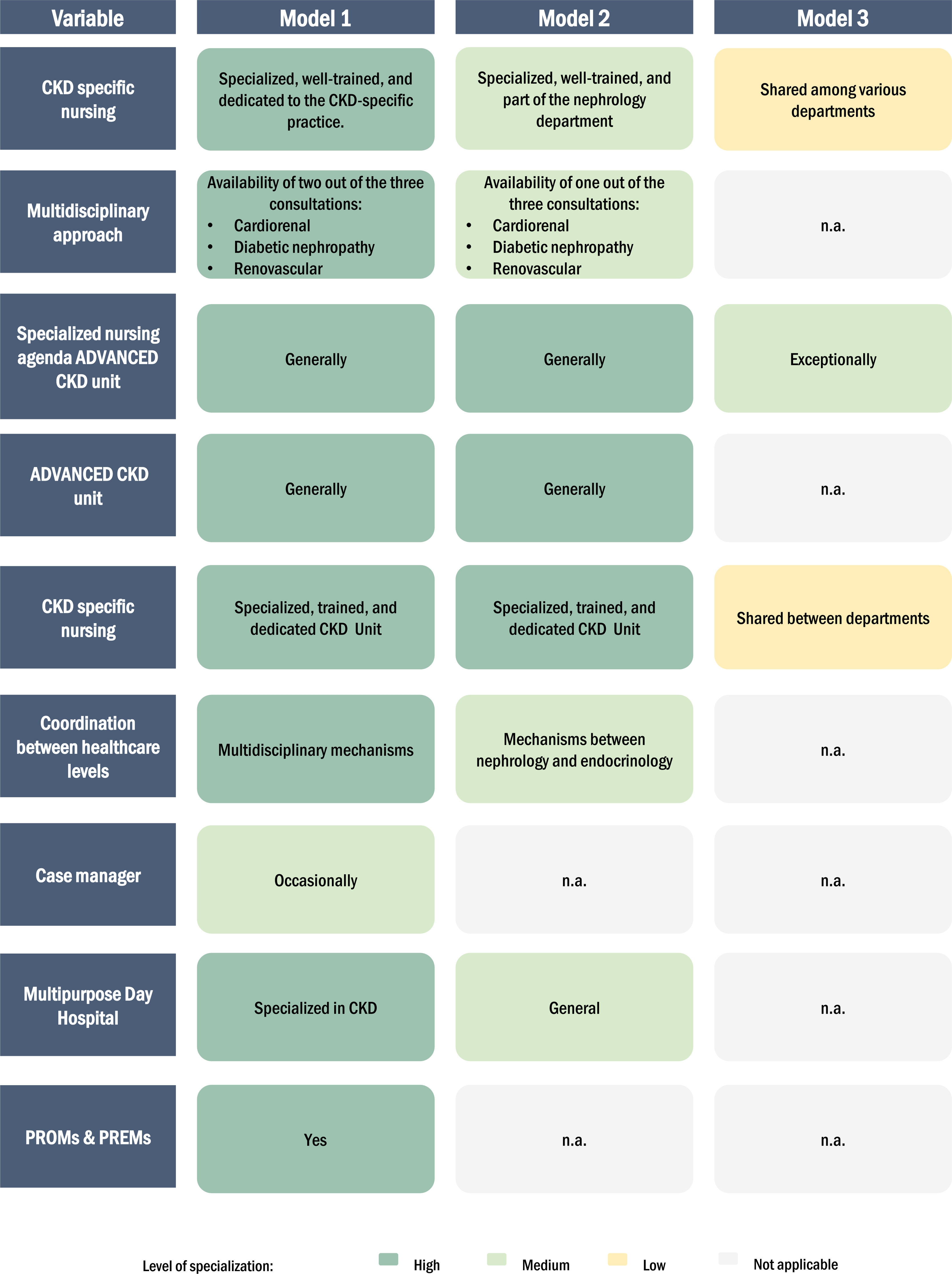
ResultsCoordination models for the management of CKD in Spanish hospitalsDuring the pilot phase conducted in five centers, three CKD patient care models were identified based on nine variables used for characterizing the different models of approach (Fig. 2). These variables were associated with the type and level of coordination among the medical specialties involved in CKD care, the roles of the professionals involved, and the availability of specific resources. A total of nine variables were identified and analyzed for the characterization of each model: (1) coordination model or multidisciplinary approach among specialties integrating nephrology, endocrinology and/or cardiology; (2) availability of skilled CKD nursing staff; (3) availability of specialized nursing care with dedicated schedules; (4) availability of advanced multidisciplinary CKD units; (5) presence of specialized nursing staff, trained and dedicated to patient care in multidisciplinary CKD units; (6) coordination, referral protocols and channels of communications among levels of care; (7) availability of case managers for managing hospital transitions, admissions and discharges); (8) availability of a multipurpose day hospital area with high specialization in CKD; and (9) availability of tools to assess patient outcomes (Patient-Reported Experience Measures [PREMs] and Patient-Reported Outcomes Measures [PROMs]).
Among three CKD patient care models, the main differentiating factor was the availability of multidisciplinary CKD units and specialized CKD nursing. Diversity and accessibility of resources for addressing CKD were differentiating factors among the models (Fig. 2). Additionally, a detailed description of the patient journey according to the phase of the care process (diagnosis, treatment, and follow-up) was described in Supplementary Material.
In Model 1, CKD units, multidisciplinary units are in place for cardiorenal and diabetic nephropathy care (renovascular unit optional) provided by specialized and trained nursing staff working in multidisciplinary units for CKD care that are adequately equipped with the necessary resources.
In Model 2, CKD units are characterized by the presence of at least one of the three multidisciplinary units mentioned: cardiorenal, diabetic nephropathy, or renovascular care. This model has a nephrology-specific nursing staff, exclusively dedicated to the care of patients with CKD (at any stage, including advanced CKD treated in multidisciplinary units). It is important to note that the nursing staff has a separate physical space and a dedicated schedule to attend to CKD patients.
Model 3 is distinguished by the fact that the nursing staff who care for CKD patients lack specific specialization, and only exceptionally have their own physical space and dedicated schedules.
Regarding communication between levels of healthcare and among specialties, models 1 and 2 differed in that the first proposes a multidisciplinary approach with bidirectional communication channels, while the second proposes “coordination between specialties”. Furthermore, Model 1 includes a multipurpose day hospital exclusively and specifically for the use of the Nephrology Unit, while in Model 2, the general hospital day unit is used. Lastly, Model 1 suggested the occasional presence of a case manager and the collection of PROMS and PREMS, features that were not available in either Model 2 or Model 3.
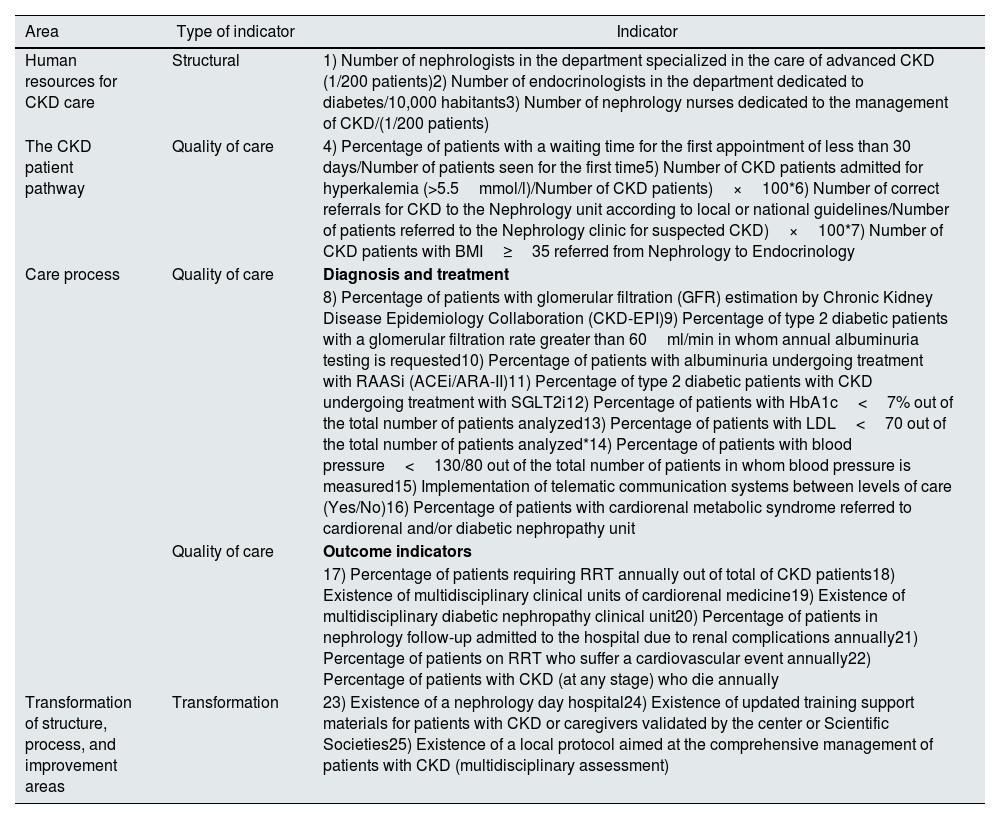
Healthcare quality indicators for the evaluation of CKD care modelsThe proposed indicators for evaluating the care provided in the CKD process in each unit include structural, quality of care, and transformation indicators (Table 1) (detailed in the materials and methods).
Structural, quality-of-care and transformation indicators validated in the CARABELA-CKD initiative according to type.
| Area | Type of indicator | Indicator |
|---|---|---|
| Human resources for CKD care | Structural | 1) Number of nephrologists in the department specialized in the care of advanced CKD (1/200 patients)2) Number of endocrinologists in the department dedicated to diabetes/10,000 habitants3) Number of nephrology nurses dedicated to the management of CKD/(1/200 patients) |
| The CKD patient pathway | Quality of care | 4) Percentage of patients with a waiting time for the first appointment of less than 30 days/Number of patients seen for the first time5) Number of CKD patients admitted for hyperkalemia (>5.5mmol/l)/Number of CKD patients)×100*6) Number of correct referrals for CKD to the Nephrology unit according to local or national guidelines/Number of patients referred to the Nephrology clinic for suspected CKD)×100*7) Number of CKD patients with BMI≥35 referred from Nephrology to Endocrinology |
| Care process | Quality of care | Diagnosis and treatment |
| 8) Percentage of patients with glomerular filtration (GFR) estimation by Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI)9) Percentage of type 2 diabetic patients with a glomerular filtration rate greater than 60ml/min in whom annual albuminuria testing is requested10) Percentage of patients with albuminuria undergoing treatment with RAASi (ACEi/ARA-II)11) Percentage of type 2 diabetic patients with CKD undergoing treatment with SGLT2i12) Percentage of patients with HbA1c<7% out of the total number of patients analyzed13) Percentage of patients with LDL<70 out of the total number of patients analyzed*14) Percentage of patients with blood pressure<130/80 out of the total number of patients in whom blood pressure is measured15) Implementation of telematic communication systems between levels of care (Yes/No)16) Percentage of patients with cardiorenal metabolic syndrome referred to cardiorenal and/or diabetic nephropathy unit | ||
| Quality of care | Outcome indicators | |
| 17) Percentage of patients requiring RRT annually out of total of CKD patients18) Existence of multidisciplinary clinical units of cardiorenal medicine19) Existence of multidisciplinary diabetic nephropathy clinical unit20) Percentage of patients in nephrology follow-up admitted to the hospital due to renal complications annually21) Percentage of patients on RRT who suffer a cardiovascular event annually22) Percentage of patients with CKD (at any stage) who die annually | ||
| Transformation of structure, process, and improvement areas | Transformation | 23) Existence of a nephrology day hospital24) Existence of updated training support materials for patients with CKD or caregivers validated by the center or Scientific Societies25) Existence of a local protocol aimed at the comprehensive management of patients with CKD (multidisciplinary assessment) |
ACEi/ARA-II: angiotensin converting enzyme inhibitors/angiotensin II receptor antagonists; ACKD: advanced chronic kidney disease; BP: blood pressure; CKD-EPI: Chronic Kidney Disease Epidemiology Collaboration; SGLT2i: sodium-glucose cotransporter-2 inhibitors; LDL: low-density lipoprotein; RAASi: Renin–angiotensin–aldosterone system inhibitors; RRT: renal replacement therapy.
A total of 156 potential indicators were initially proposed by the members of the Scientific Committee. These subsequently underwent a voting process to prioritize and select the most appropriate, and finally, the selected indicators were shared and voted on using Delphi methodology at the National Multidisciplinary Workshop and further validated in regional meetings and by the Scientific Committees. The selection criteria were feasibility of implementation and potential beneficial impact for improving patient care or healthcare results. Twenty-five indicators were selected in a two-round Delphi process at the National Workshop by 100 clinical experts. The selected indicators were presented to participants at the four Regional Multidisciplinary Meetings, in which healthcare professionals from across the country provided their feedback. The final list was confirmed by the Scientific Committee (Table 1).
The category of structural indicators focuses on how the center is organized for the management of CKD (Table 1). Healthcare quality indicators were divided according to the phase of the CKD care process: diagnosis, treatment, and follow-up (Table 1). Likewise, the Scientific Committees defined different types of transformation indicators that would offer a comprehensive view of the evolution of the care model: transformation of the structure, transformation of the process, and improvement areas.
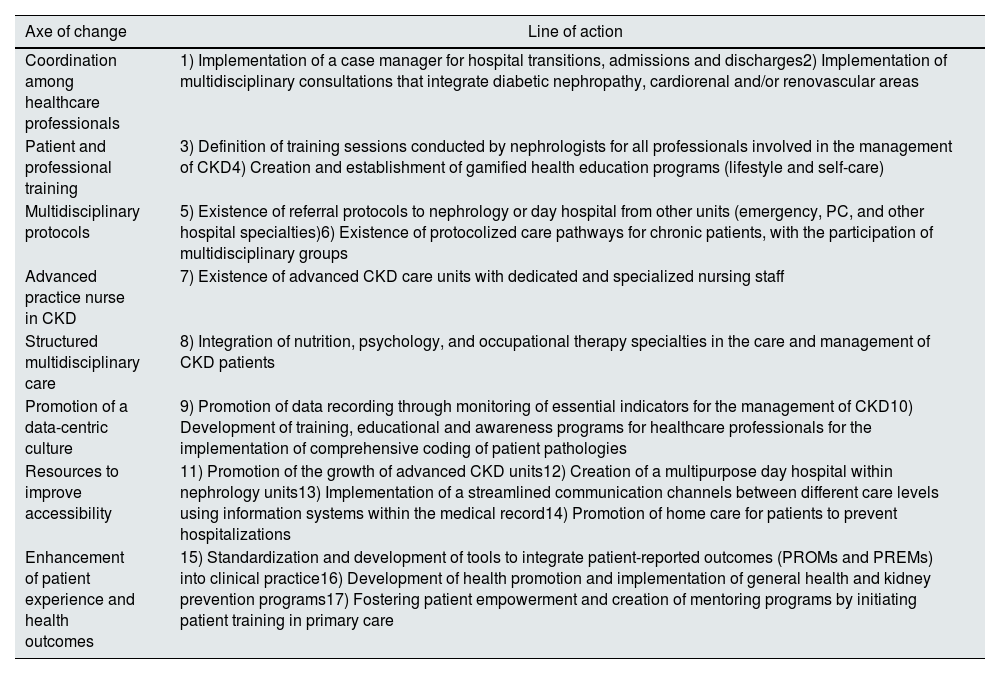
Future improvement areas for the evolution of CKD care models: barriers and potential solutionsThe comprehensive analysis identified improvement areas, which were validated in the CARABELA-CKD National Multidisciplinary Workshop. They were grouped as four major challenges: care process, social, technological, and organizational and economic solutions, all of which will be addressed in the future to establish an integrated care model.
These improvement areas were also discussed and validated at the Regional Multidisciplinary Meetings with healthcare professionals, identifying solutions (grouped as eight axes of change and 17 lines of action) (Table 2). The professional analysis and expert opinions that led to this list will be the topic of a dedicated publication.
Potential solutions identified in the CARABELA-CKD initiative.
| Axe of change | Line of action |
|---|---|
| Coordination among healthcare professionals | 1) Implementation of a case manager for hospital transitions, admissions and discharges2) Implementation of multidisciplinary consultations that integrate diabetic nephropathy, cardiorenal and/or renovascular areas |
| Patient and professional training | 3) Definition of training sessions conducted by nephrologists for all professionals involved in the management of CKD4) Creation and establishment of gamified health education programs (lifestyle and self-care) |
| Multidisciplinary protocols | 5) Existence of referral protocols to nephrology or day hospital from other units (emergency, PC, and other hospital specialties)6) Existence of protocolized care pathways for chronic patients, with the participation of multidisciplinary groups |
| Advanced practice nurse in CKD | 7) Existence of advanced CKD care units with dedicated and specialized nursing staff |
| Structured multidisciplinary care | 8) Integration of nutrition, psychology, and occupational therapy specialties in the care and management of CKD patients |
| Promotion of a data-centric culture | 9) Promotion of data recording through monitoring of essential indicators for the management of CKD10) Development of training, educational and awareness programs for healthcare professionals for the implementation of comprehensive coding of patient pathologies |
| Resources to improve accessibility | 11) Promotion of the growth of advanced CKD units12) Creation of a multipurpose day hospital within nephrology units13) Implementation of a streamlined communication channels between different care levels using information systems within the medical record14) Promotion of home care for patients to prevent hospitalizations |
| Enhancement of patient experience and health outcomes | 15) Standardization and development of tools to integrate patient-reported outcomes (PROMs and PREMs) into clinical practice16) Development of health promotion and implementation of general health and kidney prevention programs17) Fostering patient empowerment and creation of mentoring programs by initiating patient training in primary care |
CKD: chronic kidney disease; PC: primary care; PREM: patient-reported experiences; PROM: patient-reported outcomes.
CKD is a complex condition often overlooked in its early stages.6 Hence, there is an urgent need to design a coordinated strategy aimed at improving the management of individuals with CKD to implement the most effective approach for reducing mortality and healthcare expenses.11 Effective management should include addressing CKD risk factors10 and associated conditions and comorbidities12 to prevent disease progression. Indeed, a few years ago, the Commitment to Quality project led by the Spanish Society of Nephrology (S.E.N.), in coordination with the Ministry of Health, Consumption and Social Welfare, set four objectives and solutions aimed at addressing CKD comprehensively. These solutions focus on early-stage disease identification and commit to delivering high-quality, patient-centered care throughout the patient journey, starting from the initial symptoms and encompassing all stages of CKD and clinical progression.7,8,11,13
Nonetheless, the current state of the care process in our country is exceptionally diverse, reflecting a range of scenarios in the management of CKD patients. This diversity is influenced by factors such as geographical location, cultural considerations, and the distinctive characteristics of the various regional health systems.9 Consequently, it has become imperative to assess the implementation of quality-of-care programs and gain a comprehensive understanding of the current management of CKD in Spanish healthcare centers. Hence, CARABELA-CKD has concentrated its efforts on not only identifying models, but also assessing resource utilization and management characteristics. Only through this approach can we identify limitations, transform the system toward adopting effective and efficient organization and approaches, and develop targeted solutions that may be either traditional or innovative.
The results from the CARABELA-CKD in-depth characterization process conducted in five pilot centers shed light on the distinct scenarios and on the diverse levels of accessibility to resources within the management of CKD. This research has identified three care models for patients with CKD in Spanish hospitals categorized according to specialization, availability of resources, multidisciplinary care, and specialized nursing. In these models, the most significant and impactful factor is multidisciplinary collaboration, embodied by functional units, adequately equipped with the necessary resources for the management of CKD. Nonetheless, each of these models has the potential for improvement and the attainment of excellence. Additionally, a diverse set of indicators, encompassing structural, quality-of-care and transformation indicators were collected and validated to help enhance the CKD care process. These indicators provide valuable insights into critical aspects of care, enabling ongoing monitoring and guiding continuous improvement efforts.12 They are tailored to each of the identified care models and processes, thus facilitating improvements within each model that align with its distinct realities, requirements, and available resources. These improvements include effective communication and coordination among all healthcare professionals managing CKD, the promotion of education and training for both healthcare professionals and the patients themselves, and the use of protocols that incorporate referral criteria to standardize CKD care. In this regard, we draw upon previous experience from other countries, where the implementation of integrated programs has yielded notable enhancements and improvements in the care of various clinical entities.14–16
When compared with other strategic initiatives, CARABELA-CKD is an innovative proposition that takes into account the diverse realities and existing care models across Spain.9 It envisions the care of CKD patients in Spain as a circular and multidisciplinary process, involving the seamless integration of hospital care areas, such as nephrology, endocrinology, cardiology, and primary care, all operating cohesively within a patient-centered framework. This is due to the ability of the initiative to furnish a comprehensive, holistic and pragmatic perspective across various settings and scenarios, along with a tailored improvement framework that adapts to diverse contexts. Moreover, CARABELA-CKD represents a collaborative initiative that brings together both Scientific Societies and AstraZeneca, uniting clinical leadership with an integrative philosophy.
Throughout the development of this initiative, participants have evaluated, deliberated, and critically scrutinized care models and indicators, identified improvement areas, and proposed potential solutions. The participation of Scientific Societies from different specialties and healthcare professionals directly involved in the care of patients with CKD, both at the national and regional levels, adds value to this initiative.
Finally, in a subsequent practical phase, the dissemination and implementation of this initiative in the form of local workshops held in healthcare centers throughout the country will facilitate its implementation and bring about a transformation in the current care model for renal patients.
Since the CARBELA-CKD provides a robust methodology that enables each healthcare center or team to position itself within each specific model, it offers the potential for enhancement while aligning meticulously with the demands of real-world healthcare processes. In essence, each model can discern its unique reference point for improvement. Thus, through self-analysis, they can craft their own improvement plans, tailored to their individual circumstances. This transformation aims to optimize clinical pathways and the overall management of patients, ultimately leading to improved healthcare outcomes and reducing the burden of CKD.
ConclusionsIn conclusion, the CARABELA-CKD initiative is a collaborative effort, involving different Scientific Societies, healthcare professionals across Spain, and AstraZeneca. CARABELA-CKD has defined a variety of existing CKD care models which can be grouped into three main models. It has also identified strategic healthcare quality indicators in the renal patient care pathway, and has established improvement areas, applicable to all care models, and actions to be taken to enhance the quality of care for CKD. Its implementation may result in overall improvement in patient health outcomes and efficiency throughout the Healthcare Service.
FundingAll support for the present manuscript was provided by AstraZeneca Farmacéutica Spain.
Conflicts of interestMS has received payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Baxter, GSK, Boehringer, Astellas, AstraZeneca, and Vifor; has received support for attending meetings and/or travel from Vifor and Menarini; and has receipt of equipment, materials, drugs, medical writing, gifts or other services from Vifor and GSK. PR declares no conflict of interest. JID is an employee at the Medical Department of AstraZeneca Farmacéutica Spain. MPM has received grants or contracts from Sanofi; has received payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from AstraZeneca, Novo Nordisk, Lilly, Sanofi, Abbott, Boehringer, Bayer, and Menarini.
The authors acknowledge the participation of all the professionals attending the regional meetings of the CARABELA-CKD initiative and all those involved in the pilot phase, from Hospital Clínico Universitario de Valencia (Valencia, Spain), Hospital Universitario de Cruces (Vizcaya, Spain), Hospital Universitario 12 de Octubre (Madrid, Spain), Hospital Universitario Reina Sofía (Córdoba, Spain), Hospital Universitario Vall d’Hebron (Barcelona, Spain), Hospital Universitario Lucus Augusti (Lugo, Spain), Complejo Hospitalario Universitario de A Coruña (A Coruña, Spain), Hospital Universitario Marqués de Valdecilla (Santander, Spain), Hospital Universitario de Bellvitge (Barcelona, Spain), Hospital Universitario Juan XXIII (Tarragona, Spain), Hospital Universitario Doctor Josep Trueta (Girona, Spain), Hospital Universitario Fundación Jiménez Díaz (Madrid, Spain), Centro de Salud Rafael Alberti (Madrid, Spain), Hospital Universitario Virgen de las Nieves (Granada, Spain), Hospital Universitario Virgen Macarena (Seville, Spain), Hospital Universitario de Badajoz (Badajoz, Spain).
Medical writing support under the guidance of the authors was provided by Laura Vilorio Marqués, PhD, Blanca Piedrafita, PhD, and Javier Arranz-Nicolás, PhD, from Medical Statistics Consulting (MSC), Valencia, Spain, in accordance with Good Publication Practice guidelines (DeTora, L.M. et al. Ann Intern Med. 2022).
The CARABELA-CKD Scientific Committee consists of the following members: Borja Quiroga (Sociedad Española de Nefrología, S.E.N.), Javier Escalada (Sociedad Española de Endocrinología y Nutrición, SEEN), Juan José Gorgojo (SEEN), Manuel Pérez Maraver (SEEN), Mercedes Salgueira (S.E.N.), Patricia de Sequera (S.E.N.), Pedro Ruiz (Sociedad Española de Calidad Asistencial), Alberto Prado Dominguez (AstraZeneca Farmacéutica Spain), Jesús Ignacio Diago (AstraZeneca Farmacéutica Spain), and Lucía Regadera (AstraZeneca Farmacéutica Spain).