Chronic kidney disease (CKD) is associated with high cardiovascular disease (CVD) risk, and requires specific interventions to decreases CVD risk.
The guidelines indicate that systematic global CVD risk assessment is recommended in individuals with any major vascular risk factor. The European Society Cardiology (ESC) guidelines, he European Renal Association (ERA) Council and the Spanish Society of Nephrology (S.E.N.) in collaboration with 15 Scientific Societies recommend assessing albuminuria in all these populations.
We have evaluated current clinical practice regarding the assessment of CVD risk factors (blood pressure, albuminuria, serum cholesterol, glycemia and creatinine) in different adult health user populations, analyzing the results separately for men and women, given recent evidence on gender differences in the recognition, monitoring, and management of CKD.
MethodsObservational, retrospective, non-interventional single center study performed in a hospital using Electronic Health Record (EHR) data.
ResultsAmong 707,493 healthcare users, 612,619 were adults, and of these 332,943 (54.3%) females; 73,632 (12.0%) had DM and 121,445 (19.8%) hypertension. Mean (SD) age was 68.91±21.4 years; 261,694 (36.9%) were older than 50 years.
Only 8522 (1.39%) had undergone albuminuria testing as compared with 264,684 (43.21%) tested for serum creatinine, 140,492 (22.93%) for serum cholesterol, 263,381 (42.99%) for serum glucose, and 226,448 (36.96%) for blood pressure. Albuminuria was the only cardiovascular risk factor assessed more frequently in men than in women.
Albuminuria, as other CVD risk factors, was more frequently assessed in patients with DM (6.71% of patients) or hypertension (4.81%), but albuminuria assessment remained suboptimal compared with 58–87% for other cardiovascular risk factors. For adults with diabetes or hypertension, albuminuria was assessed more frequently in men than in women.
Albuminuria assessment in those older than 50 years was also suboptimal at 2.24%, as compared with 31–47% for other CVD risk factors.
Albuminuria and EGFR are needed to screen for CKD, meaning that a urine test for albumin and creatinine and a serum test for creatinine are needed. To these, we may add assessment of blood pressure, serum cholesterol (for familial hypercholesterolemia) and serum glucose for Diabetes. Albuminuria was the only cardiovascular risk factor that was assessed more frequently in men (up to nearly 60% more frequently), indicating that screening for CKD and CVD risk in women is suboptimal. This result is surprisingly consistent across time and in all age groups. This is the first time that gender disparities in the assessment of albuminuria have been revealed.
ConclusionAlbuminuria is assessed infrequently, even in patients with a high cardiovascular risk, especially in women.
La enfermedad renal crónica (ERC) se asocia con un alto riesgo de enfermedad cardiovascular (ECV) y requiere intervenciones específicas para disminuir este riesgo.
Las guías recomiendan una evaluación global sistemática del riesgo de ECV en personas con cualquier factor de riesgo vascular importante. Las guías de la Sociedad Europea de Cardiología (SEC), la Asociación Renal Europea (ERA) y la Sociedad Española de Nefrología (SEN), en colaboración con 15 sociedades científicas, recomiendan evaluar la albuminuria en todas estas poblaciones.
Hemos evaluado la práctica clínica actual con respecto a la evaluación de los factores de riesgo de ECV (presión arterial, albuminuria, colesterol sérico, glucemia y creatinina) en diferentes poblaciones adultas de usuarios de salud, analizando los resultados por separado para los hombres y las mujeres, dada la evidencia reciente sobre las diferencias de género en el reconocimiento, el seguimiento y el tratamiento de la ERC.
MétodosEstudio observacional, retrospectivo, no intervencionista, unicéntrico, realizado en un hospital utilizando datos de la historia clínica electrónica.
ResultadosDe los 707.493 usuarios de atención sanitaria, 612.619 eran adultos. De ellos, 332.943 (54,3%) eran mujeres, 73.632 (12,0%) tenían DM y 121.445 (19,8%) tenían hipertensión. La edad media (DE) fue 68,91 ± 21,4 años; 261.694 (36,9%) eran mayores de 50 años.
Solo 8.522 (1,39%) se habían sometido a pruebas de albuminuria en comparación con 264.684 (43,21%) de creatinina sérica, 140.492 (22,93%) de colesterol sérico, 263.381 (42,99%) de glucosa sérica y 226.448 (36,96%) de presión arterial. La albuminuria fue el único factor de riesgo cardiovascular evaluado con mayor frecuencia en hombres que en mujeres.
La albuminuria, como otros factores de riesgo de ECV, se evaluó con mayor frecuencia en pacientes con DM (6,71% de los pacientes) o hipertensión (4,81%), pero la evaluación de la albuminuria siguió siendo subóptima en comparación con el 58% al 87% para otros factores de riesgo cardiovascular. Para los adultos con diabetes o hipertensión, la albuminuria se evaluó con mayor frecuencia en hombres que en mujeres.
La evaluación de la albuminuria en los mayores de 50 años también fue subóptima, con un 2,24%, en comparación con un 31% a un 47% para otros factores de riesgo de ECV.
La albuminuria y el FGe son necesarios para detectar ERC, lo que implica la determinación de albúmina y creatinina en orina y de creatinina en suero. A estos podemos agregar la evaluación de la presión arterial, el colesterol sérico (para la hipercolesterolemia familiar) y la glucosa sérica para la diabetes. La albuminuria fue el único factor de riesgo cardiovascular que se evaluó con mayor frecuencia en hombres (hasta casi un 60% más frecuentemente), lo que indica que la detección de ERC y riesgo de ECV en mujeres es subóptima. Este resultado es sorprendentemente consistente a lo largo del tiempo y en todos los grupos de edad. Esta es la primera vez que se revelan disparidades de género en la evaluación de la albuminuria.
ConclusiónLa albuminuria se evalúa con poca frecuencia, incluso en pacientes con alto riesgo cardiovascular, especialmente en mujeres.
Chronic kidney disease (CKD) is usually diagnosed based on the presence of a reduced estimated glomerular filtration rate (eGFR, <60mL/min/1.73m2) or albuminuria (urinary albumin–creatinine ratio [UACR]>30mg/g) for longer than 3 months.1 A diagnosis of CKD is associated with increased risks of progression to kidney failure and all-cause and cardiovascular death, among others.1 However, awareness of CKD diagnostic criteria outside Nephrology is limited. Recently, the 2021 European Society of Cardiology (ESC) Guidelines on cardiovascular disease (CVD) prevention in clinical practice adopted the KDIGO risk categories based on eGFR and albuminuria to define mild, moderate, and severe CKD.2 Moderate or severe CKD are associated with high and very high CVD risk, respectively, and require specific interventions to decreases CVD risk, independently from the presence of other CVD risk factors. An algorithm on CVD prevention provided in the guidelines starts by assessing whether the patient has established CVD, CKD, diabetes mellitus (DM) or familial hypercholesterolemia, implying that serum glucose, serum cholesterol, eGFR and albuminuria should be part of the baseline assessment for CVD risk. Furthermore, the guidelines indicate that systematic global CVD risk assessment is recommended in individuals with any major vascular risk factor (i.e., family history of premature CVD, familial hypercholesterolemia, CVD risk factors such as smoking, hypertension, DM, hyperlipidemia, obesity, or comorbidities increasing CVD risk). Additionally, systematic or opportunistic CVD risk assessment in the general population men>40 years and women>50 years or postmenopausal with no known CVD risk factors may be considered. De facto, the ESC guidelines recommend or suggest assessing albuminuria (a requirement to exclude CKD) in all these populations, a feature recently emphasized by the European Renal Association (ERA) Council and the Spanish Society of Nephrology (SENEFRO) in collaboration with 15 Scientific Societies.3,4 Baseline and periodic assessment of albuminuria has also been recommended for patients with DM or hypertension for over 20 years.5,6
The next logical step is to act, favoring the implementation of Clinical Guidelines. A key element of implementation is the evaluation of current clinical practice, to diagnose the initial situation, identify areas most in need of improvement and establish corrective measures and goals that can be evaluated in repeated cycles of continuous improvement processes. However, the starting point in Spain, a representative Western Europe country projected to have the longest life expectancy in the world by 2040, is unknown, although there is anecdotal evidence of suboptimal implementation of albuminuria assessment outside the fields of nephrology and diabetes.
We have now evaluated current clinical practice regarding the assessment of CVD risk factors (blood pressure and laboratory parameters such as albuminuria, serum cholesterol, glycemia and creatinine to assess estimated glomerular filtration rate) in different adult health user populations, analyzing the results separately for men and women, given recent evidence on gender differences in the recognition, monitoring, and management of CKD.7
MethodsAn observational, retrospective, non-interventional single center study was performed in a Spanish teaching hospital using Electronic Health Record (EHR) data.
The study includes clinical data collected between January 1st 2011, and October 31st 2022, which apply to a total of 707,493 patients, of whom 612,609 were older than 18 years and more than 63,000,000 documents. Data comes from documents generated in the Outpatient, Hospitalization and Emergencies areas from all departments of the Infanta Leonor University Hospital, as well as laboratory, pharmacy (hospital and oncological), radiology, pathology and microbiology data. The Infanta Leonor University Hospital is a computerized second level University Hospital, which provides specialized health care services to a population of more than 300,000 in the southeast of Madrid. EHR are accessed by the computer solution SELENE, that does not include primary care data.8 Using Artificial Intelligence (AI), Machine Learning (ML) and Deep Learning (DL) techniques, specifically those applied to Natural Language Processing (NLP), the information was extracted from the EHRs and analyzed using the Savana software Manager v4.0 (SMv4) developed by Medsavana, S.L. (hereinafter Savana).9 SMv4 allows interpreting and exploiting the clinical information found in medical records, converting the data generated in the hospital, including the information contained in the free text, into structured and reusable data for research purposes.10–12
The first phase to build the structured database consisted of data acquisition. This phase was the responsibility of the medical center, which collaborates with Savana technical staff to pseudonymize the data and transfer it to Savana, using a secure file transfer protocol (SFTP). In a subsequent phase of integration, the EHRs are included in an inventory that is being prepared for the NLP phase, in which the EHRead® technology developed by Savana is used. This stage includes standardizing the EHR format, cleaning the data, and preparing reports on their quality. EHRead® technology uses NLP techniques to extract pseudonymous EHR free text clinical variables and shape the structured database.
The information was extracted from the free text, recognizing the clinical variables of interest, as well as their attributes, denials and temporality. The list of variables to be extracted from the unstructured text was decided jointly by the research team and Savana staff to ensure accuracy and detection sensitivity. These variables are detailed below:
- 1.
Clinical variables: age, sex, year of assessment, diabetes, arterial hypertension, chronic kidney disease. The terms included for the analysis of each of the variables were Diabetes, including type 1 and type 2 (diabetes mellitus, diabetes, DBT, DM, DMID, diabetic), hypertension (HTA, arterial hypertension, hypertensive vascular disease, hypertensive disease (excluding pulmonary, portal, ocular)) and chronic kidney disease (CKD, CRD, chronic renal dysfunction, chronic kidney disease, chronic renal failure, chronic renal function impairment). These terms and the acronyms were searched for in Spanish.
- 2.
Analytical variables (extracted from structured laboratory data): albuminuria or urine albumin (urinary albumin/creatinine ratio, 24-h urine albumin excretion), urine creatinine, blood creatinine, blood glucose, blood cholesterol and blood pressure.
The data were analyzed, obtaining the percentages of all patients who had determinations of albuminuria, cholesterol, glycemia, estimated glomerular filtration rate (eGFR) and measurement of blood pressure. The prevalence of these data was analyzed in the total population studied and also in subgroups based on age, gender, and hypertension and diabetes status.
The present study was approved by the Clinical Research Ethics Committee of the Infanta Leonor University Hospital (code PI 047-23).
Statistical analysisTwo-sided p<.05 was considered statistically significant. All analyses were conducted using R software (RStudio Version 1.2.5033).
ResultsAmong 707,493 healthcare users, 612,619 were adults, and of these 332,943 (54.3%) females; 73,632 (12.0%) had DM and 121,445 (19.8%) hypertension. Mean (SD) age was 68.91±21.4 years; 261,694 (36.9%) were older than 50 years.
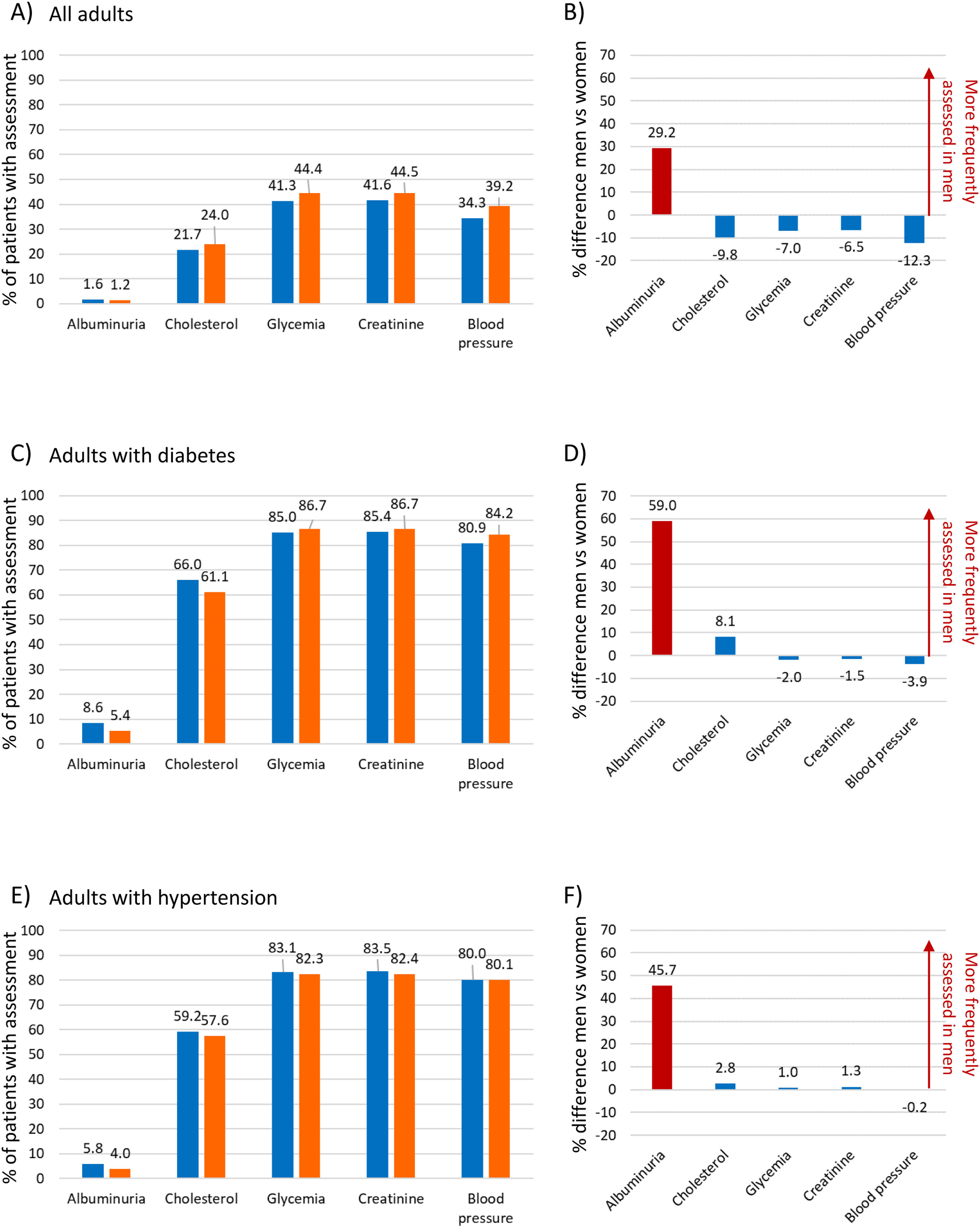
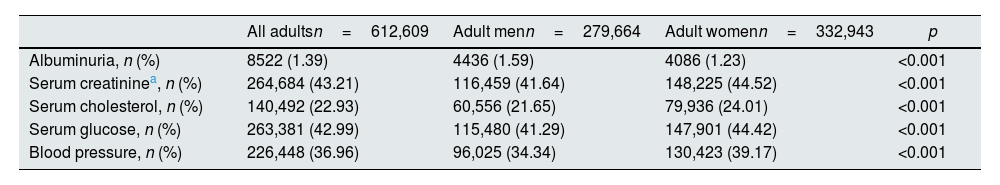
Table 1 shows the percentage of adults with at least one assessment of different cardiovascular risk factors: only 8522 (1.39%) had undergone albuminuria testing as compared with 264,684 (43.21%) tested for serum creatinine, 140,492 (22.93%) for serum cholesterol, 263,381(42.99%) for serum glucose, and 226,448 (36.96%) for blood pressure. Albuminuria was the only cardiovascular risk factor assessed more frequently in men than in women (Fig. 1A, B) in all age groups.
Adults with at least one assessment of cardiovascular risk factors among all adults and by gender.
| All adultsn=612,609 | Adult menn=279,664 | Adult womenn=332,943 | p | |
|---|---|---|---|---|
| Albuminuria, n (%) | 8522 (1.39) | 4436 (1.59) | 4086 (1.23) | <0.001 |
| Serum creatininea, n (%) | 264,684 (43.21) | 116,459 (41.64) | 148,225 (44.52) | <0.001 |
| Serum cholesterol, n (%) | 140,492 (22.93) | 60,556 (21.65) | 79,936 (24.01) | <0.001 |
| Serum glucose, n (%) | 263,381 (42.99) | 115,480 (41.29) | 147,901 (44.42) | <0.001 |
| Blood pressure, n (%) | 226,448 (36.96) | 96,025 (34.34) | 130,423 (39.17) | <0.001 |
p values are provided for the comparison between men and women.
Percentage of patients with at least one assessment of diverse cardiovascular risk factors. (A) All adult healthcare users. (B) Difference between men and women in the assessment of diverse cardiovascular risk factors for all adult healthcare users, expressed as percentual difference. (C) Adults with a diagnosis of diabetes. (D) Difference between men and women in the assessment of diverse cardiovascular risk factors for adults with diabetes, expressed as percentual difference. (E) Adults with hypertension. (F) Difference between men and women in the assessment of diverse cardiovascular risk factors for adults with hypertension, expressed as percentual difference.
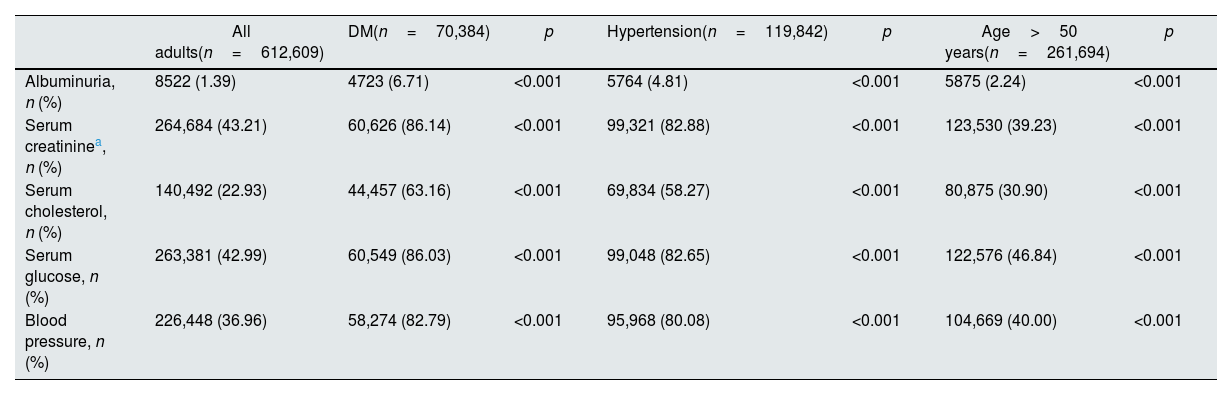
Albuminuria, as other CVD risk factors, was more frequently assessed in patients with DM (6.71% of patients) or hypertension (4.81%), but albuminuria assessment remained suboptimal compared with 58–87% for other cardiovascular risk factors (Table 2). For adults with diabetes (Fig. 1C, D) or hypertension (Fig. 1E, F), albuminuria was assessed more frequently in men than in women, respectively, whereas gender differences for other risk factors remained below 10%. Albuminuria assessment in those older than 50 years was also suboptimal at 2.24%, as compared with 31–47% for other CVD risk factors.
Adults with at least one assessment of cardiovascular risk factors among all adults and by comorbidities and older age.
| All adults(n=612,609) | DM(n=70,384) | p | Hypertension(n=119,842) | p | Age>50 years(n=261,694) | p | |
|---|---|---|---|---|---|---|---|
| Albuminuria, n (%) | 8522 (1.39) | 4723 (6.71) | <0.001 | 5764 (4.81) | <0.001 | 5875 (2.24) | <0.001 |
| Serum creatininea, n (%) | 264,684 (43.21) | 60,626 (86.14) | <0.001 | 99,321 (82.88) | <0.001 | 123,530 (39.23) | <0.001 |
| Serum cholesterol, n (%) | 140,492 (22.93) | 44,457 (63.16) | <0.001 | 69,834 (58.27) | <0.001 | 80,875 (30.90) | <0.001 |
| Serum glucose, n (%) | 263,381 (42.99) | 60,549 (86.03) | <0.001 | 99,048 (82.65) | <0.001 | 122,576 (46.84) | <0.001 |
| Blood pressure, n (%) | 226,448 (36.96) | 58,274 (82.79) | <0.001 | 95,968 (80.08) | <0.001 | 104,669 (40.00) | <0.001 |
p values are provided for the comparison between patients with and without each comorbidity or age category.
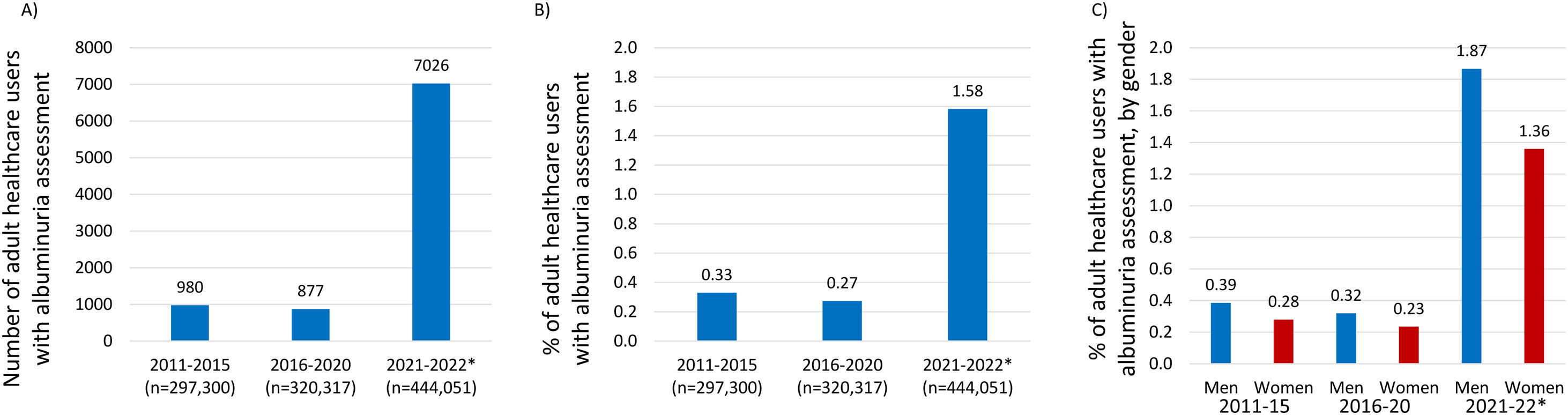
Over time (Fig. 2), statistically significant differences were observed in the assessment of albuminuria. In the most recent two years (2021–2022), albuminuria assessment was higher than in the previous decade (2011–2020), but the gap between men and women increased.
DiscussionCKD is a major amplifier of cardiovascular risk. The hallmarks of CKD, albuminuria, low eGFR, or both, are associated with progressive increases in the risk of major atherosclerotic vascular and HF events and cardiovascular death.13,14 The heightened risk begins at the earliest stages of kidney disease, most easily recognized by the presence of albuminuria.15 This biomarker reflects global vascular endothelial dysfunction and early kidney disease, and Albuminuria as low as >2.5mg/g is already associated with an increased risk of premature death16 further amplified by traditional metabolic risk factors such as elevated blood pressure, hypercholesterolemia and hyperglycemia.
The main result is the gender difference in the low assessment rate for albuminuria either among general adult healthcare users or specific high-risk subgroups for which guidelines recommend or suggest assessment of CVD risk factors that includes albuminuria (DM, hypertension, older persons). The large genders differences in albuminuria assessment either in the general adult population or in specific risk groups differed from other CVD risk factors, as albuminuria was assessed as much as nearly 60% more frequently in men that in women. It is important to highlight, that as compared with females, males tend to have greater muscle mass and higher levels of urinary creatinine excretion. Therefore, a hypothetical female patient with lower muscle mass but equivalent daily urinary albumin excretion will have a higher ACR compared with a male counterpart. For that reason, sex specific cut-points for ACR measurements are recommended.17 In a cohort of 2,051,158 participants (54% women) from general population, while higher risk was associated with lower estimated glomerular filtration rate and higher albumin–creatinine ratio in both sexes, the slope of the risk relationship for all-cause mortality and for cardiovascular mortality were steeper in women than in men.18 In another population-based cohort of 47,714 adults in Canada, sex was the most important modifier of the relationship between ACR and PCR.19
Finally, a recent uptick in albuminuria assessment has coincided with the publication of the 2021 ESC Guidelines on CVD prevention, and of clinical trials demonstrating kidney and cardiovascular protection by sodium glucose cotransporter-2 inhibitor (SGLT2i) that had an albuminuria inclusion criterion.2,20
The results obtained in all adult users of a secondary level public hospital and its associated primary care catchment area in a low socioeconomic background neighborhood are in line with prior estimates on the underutilization of albuminuria testing even in patients with hypertension and with diabetes21 but adds novel information on gender disparities and recent trends obtained by EHRead® technology. The massive data analysis can be a useful tool to approach the health from the perspective of sex and gender, since it gives us a very valuable information from the real world and helps us detect possible inequities. Among persons with diabetes, for whom annual albuminuria testing has long been guideline-recommended, testing rates have consistently been approximately 50% or lower across a variety of settings. Albuminuria testing rates among persons with hypertension without diabetes are much lower at approximately 10%. The present data provide even lower estimates.
However, the novelty of the data lies in the assessment of gender differences and recent trends. The 2021 ESC Guidelines on CVD prevention algorithm for CVD risk estimation starts by assessing whether four conditions are present: established atherosclerotic CVD, DM, CKD, and familial hypercholesterolemia. Besides past history, from a dissemination point of view, this may be summarized as the need for physicians to assess the A, B, C, D and E.4 Albuminuria and EGFR are needed to screen for CKD, meaning that a urine test for albumin and creatinine and a serum test for creatinine are needed. To these, we may add assessment of Blood pressure, serum Cholesterol (for familial hypercholesterolemia) and serum glucose for Diabetes. Albuminuria was the only cardiovascular risk factor represented in the A, B, C, D, E that was assessed more frequently in men (up to nearly 60% more frequently), indicating that screening for CKD and CVD risk in women is suboptimal. This result is surprisingly consistent across time and in all age groups. To the best of our knowledge, this is the first time that gender disparities in the assessment of albuminuria have been revealed. The recent uptick in albuminuria testing is promising and likely related to awareness campaigns on CVD prevention and early diagnosis of CKD, once that novel therapeutic approaches are available.
This study has limitations that should be considered. The main limitations are those inherent to the use of AI tools in large databases, in which a detailed individual analysis of the subjects studied is not possible. The results obtained through these methods are limited by the medical chart heterogeneity, the unstructured language analysis, the degree to which physicians reflect their patients’ medical status accurately, and the amount of missing data.22 Another limitation is the retrospective and single center nature of the study.
The strengths include that this is the first study, to the best of our knowledge, to analyze the albuminuria assessment according to gender in a large adult population of healthcare users. Another strength is the use of real data and a large (over 700,000), unbiased sample size.
In conclusion, albuminuria is assessed infrequently, even in patients with a high cardiovascular risk, especially in women. These data may facilitate the design of awareness campaigns beyond nephrology, using easy to remember infographics, such as the A, B, C, D, E concept.
Data sharing statementData are available upon reasonable request to the authors. Subsequently, the authors, together with the hospital's Ethics Committee, will evaluate the proposal and potentially proceed to share the data.
Conflict of interestsThe authors declare that they have no conflict of interest.