The success or failure of hemodialysis (HD) as a renal replacement therapy technique depends on our ability to achieve the best vascular access (VA) for each patient.1 The ideal VA should allow a safe and continuous handling, provide sufficient flow and free of complications. In addition, it must be individualized and durable over time.
Although the perfect VA does not exist, the native arteriovenous fistula (native AV fistula) is recommended in most cases, as it is associated with longer functional access, lower infection and complication rates than prosthetic fistulas and central venous catheters (CVC), resulting in a significant reduction in morbidity and mortality and healthcare costs.1–3
There are different studies showing that the creation of interdisciplinary teams has improved the percentage of patients dialyzed with fistulas compared to those dialyzed with a catheter,4–6 and where ultrasound has played a very important role in the achievement of good results in incident patients.5,6 However, the rate of catheter use in prevalent patients was hardly modified.6
Reducing the percentage of prevalent patients with CVC is a complex task7 that varies from one center to another. Present numbers of CVC are high, around 30–40% depending on the center7–9 and geographical area.10 In addition to the problems that may arise from late referral from the Advanced Chronic Kidney Disease (ACKD) unit, or from the surgical team, one of the aspects that contributes to maintaining these figures is the refusal of patients with CVC to have an arteriovenous (AV) fistula placement; refusal rates are as high as 36%.
In a recent study of 637 prevalent patients in out-of-hospital HD units, out of 255 catheter carriers, 36% refused to have a new AV fistula,7 and the main reasons were fear and preferences for comfort and esthetics. It has been shown that starting HD with a CVC predisposes the patients to refuse an AV fistula, and this refusal increases the longer they have had the CVC,11 so one of the most important actions is not to delay the creation of an AV fistula, preferably in ACKD units.4
Multiple causes determine whether an ACKD patient accesses dialysis with CVC, such as the exacerbation of a previously stable renal disease, lack of time for the perform of AV fistula12,13 before arrival at dialysis, or the late referral to surgery or the delay of surgery because it is not considered a priority.14,15
One of the fundamental requisites for patients to start HD with an AV fistula instead of a CVC is for ACKD units to identify early on those patients with a higher risk of worsening of their renal disease (due to heart disease or diabetes mellitus, for example) and those with a risk of slow maturation or fistula complications (women, advanced age, peripheral artery disease, smoking or obesity).16,17 These are the patients who come to the HD with a catheter and subsequently refuse to have an AV fistula performed.7 The use of ultrasound allows early assessment of patients and their identification as candidates for AV fistula. It is thus possible to perform the AV fistula before difficulties may occur and allow time, for AV fistula to mature.4
Among patients who urgently start HD with a CVC, there is a high proportion of patients who have not had a follow-up and evaluation in the ACKD unit and have not undergone a joint decision-making process on the different renal replacement therapy options, nor on aspects related to VA,7 so it is essential that this information and evaluation be provided later in the HD unit.
According to some studies,7 the factors that influence the use of CVC versus AV fistula are modifiable, such as the relationship between the referral hospital and the center,7 VA management models and the relationship between vascular surgery and nephrology.18 In some places, the healthcare organization presents serious deficiencies that negatively affect VA outcomes and justify that many patients prefer to keep their catheter instead of opting for an AV fistula. These organizational deficiencies, lack of trained staff, insufficient resources or poor time and priority management lead to unjustified delays in the performance of AV fistula or poor AV fistula outcomes.19
The existence of previous AV fistula attempts generates negative experiences in patients, which influence their decision due to fear of undergoing a new surgery.7 This situation can be the the cause a vicious cycle that encourages the use of CVC in the future.7 To address this, the main objective should be to avoid the modifiable causes that lead to HD with CVC by incorporating new tools that minimize this situation.
The association between the number of previous AV fistula attempts and fear to have surgery suggests the existence of negative experiences in patients7 that influence their decision. This favors the vicious circle that initiating HD through a CVC for whatever reason will undoubtedly favor the use of CVC in the future,7 so the main objective should be to avoid the modifiable causes that lead to arrival at HD with catheter by analyzing and correcting those causes of our process that favor it and incorporating new tools that minimize this situation.
This editorial aims to delve into practices that can help decrease the high prevalence of HD patients with CVC and patient refusals to undergo AV fistula by approaching it from the perspective of the patient’s needs.
Adequate organization and planning of vascular access by ACKD unit together with vascular surgeryCommunication between the ACKD unit and vascular surgery unit is fundamental, both in the adaptation of the referral time and performance of VA as well as in the type of VA. One of the most frequent causes of refusal of AV fistula is fear due to previous negative experiences, hence the importance of choosing good, motivated, involved and experienced surgical teams. An avoidable bad experience can be vital in the subsequent survival and future of the patient.
Use of vascular Doppler ultrasound in the ACKD unitThe use of Doppler ultrasound by nephrology physicians and nephrology nursing professionals will open the possibility of a more accurate diagnosis and a more appropriate referral in time and type to surgery.
These ultrasound professionals play a leadership and coordination role of the VA team by ensuring diligence in the physician and patient’s decision-making processes, optimizing resources and ensuring economic sustainability, preventing the overload of other departments, and has an impact on the survival and viability of the VA.4,20 The inclusion of the Doppler ultrasound in the ACKD unit provides advantages in terms of optimization of time and resources, both physical (need for another ultrasound consultation-clinic) and personnel, while the patient's care needs are centralized in the ACKD team.4
New tools in ACKD units to influence refusals to FAVAs we have stated, refusals to create an AV fistula account for a significant percentage of the high prevalence of CVC. Informing a person that the best option for him or her is an AV fistula when they have decided on a catheter is not an easy task, and the patient's decision must prevail. However, we must ensure that the decision is made with full knowledge and understanding of the problem, so specific communication techniques are needed,21 as well as ensuring that the information arrives in an appropriate and adapted for each patient.
Here are the tools to implement in ACKD and HD units to address this growing problem.
Decision support toolsPatient participation in decision-making is essential to take into account their preferences. Decision support tools facilitate the dialogue between healthcare professionals and patients and are designed to teach and empower decision-making.22,23
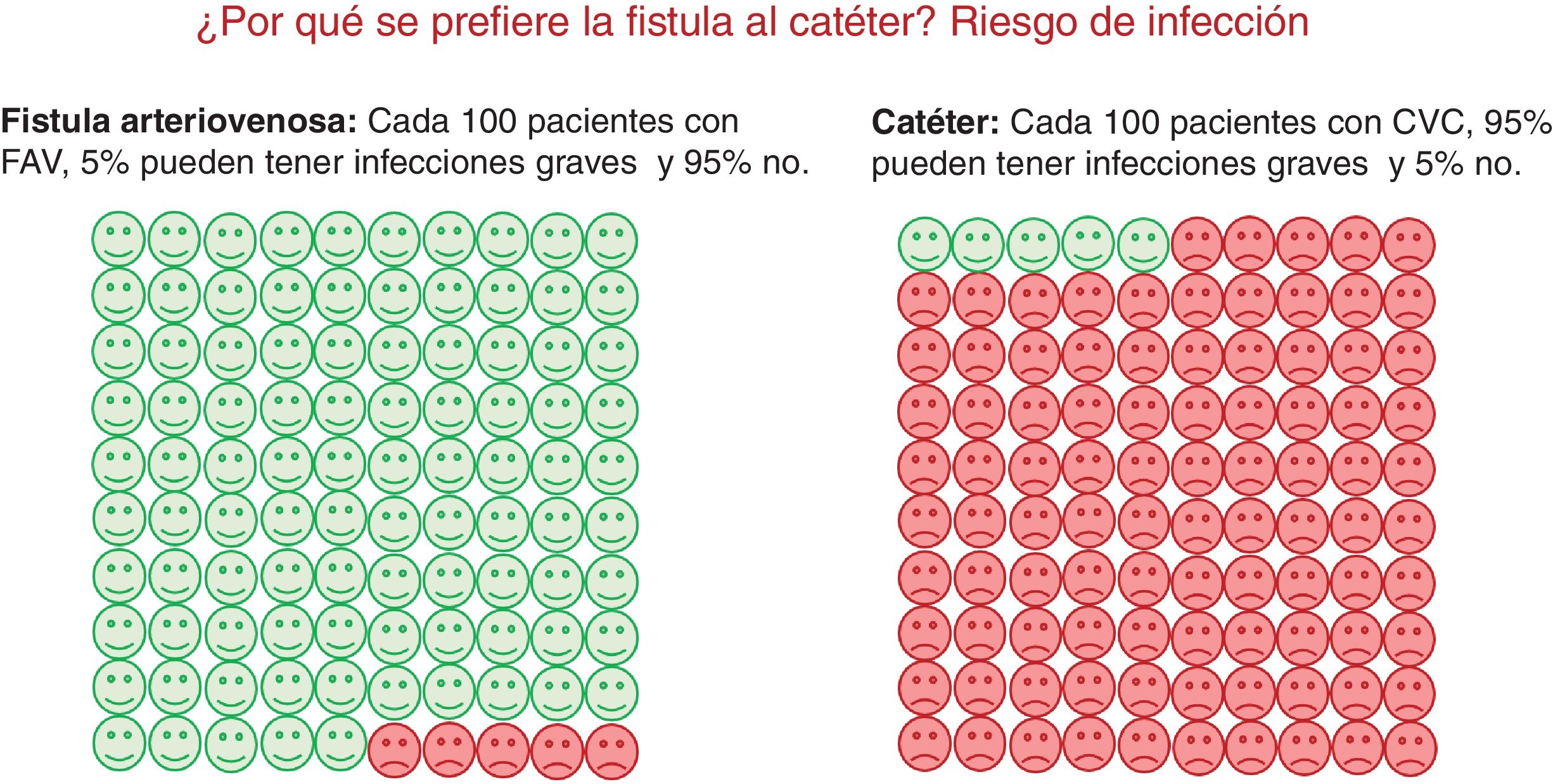
Decision-making about the best VA requires that the patient truly understands the advantages and disadvantages of each option, and that his or her doubts and fears are addressed in understandable and individually personalized language.24 Although these tools vary in content, they have in common the exposition of more than one reasonable strategy for each question regarding clinical management and it is also required a description of possible outcomes25 (Fig. 1).
Psychology professionalsThe role of the psychologist in the interdisciplinary team of the VA includes several functions, some applicable to health personnel and others to patients.
Among the actions aimed at healthcare personnel are:
- -
Advising the healthcare team on the patient's psychological factors involved in VA, i.e., what emotions and expectations may affect the patient's decision to choose one type of VA or another, as well as what emotions may be related to the choice the patient has made.
- -
Training of healthcare personnel involved in VA on how to establish a more complete relationship to help and communication with the patient, which facilitates shared decision-making based on security and knowledge, as opposed to fear and anxiety. This applies to communications in "difficult situations" or transmitting bad news.17 In these situations, negative emotions can hinder or block a more accurate decision regarding VA.
- -
Advice on which evaluation questionnaires might best fit into the procedure.
In relation to the patient, the psychologist could intervene when the causes that determine the patient's refusal to create a fistula are derived from stress as, for example, negative or traumatic experiences in the creation of the VA that may have led to phobic experiences and that may require a more specific psychological intervention, such as cognitive/behavioral therapy.26
All the work of this interdisciplinary team would not remain only in the ACKD units, but it should continue in the HD wards, working on VA decisions at all stages of kidney disease, favoring that the decision-making process go beyond the ACKD units.
ConclusionsRefusal to perform AV fistula is one of the most important aspects contributing to the maintenance of a high number of CVC in the units. A broad vision and the approach to the causes of refusals from the patient's perspective are essential to change the trend. This editorial presents new approaches that are part of a research project aiming to solve the communication barrier about vascular access by training and educating staff in both ACKD and dialysis facilities in the use of ultrasound, in psychological care in the face of refusal and fear, and in the use of decision-making tools.