We present a series of 21 patients with chronic kidney disease (CKD) on haemodialysis who were admitted due to SARS-CoV-2 infection, diagnosed by PCR of naso-oropharyngeal swab. The period of inclusion was from 11 March to 20 April 2020, monitoring the time to SARS-CoV-2 PCR negativisation. In the case of patients on a haemodialysis programme, it was necessary to monitor the SARS-CoV-2 PCR in order to decide on the period of isolation for these patients.
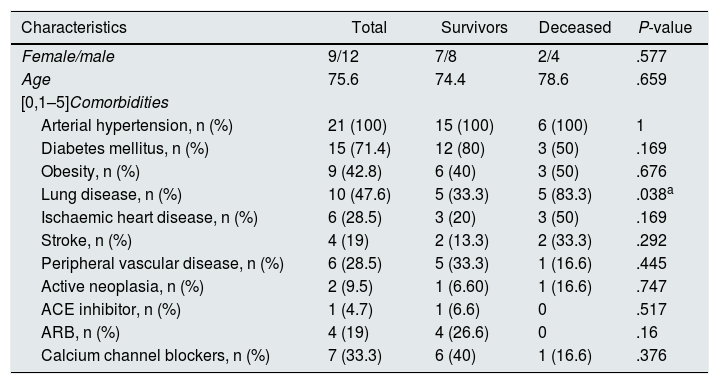
The median age was 75 years (between 50 and 89 years) with a higher prevalence of men (12 cases, 57%). Among the clinical history, all patients suffered from arterial hypertension (AHT), 15 (71%) from diabetes mellitus (DM), 9 (43%) from obesity, 10 (47%) from previous pulmonary disease, 6 (28%) from ischaemic heart disease, 6 (28%) from peripheral vascular disease, and 4 (19%) from cerebrovascular disease. Regarding antihypertensive treatment, 7 patients (33%) received calcium channel blockers, 4 (19%) ARBs, 4 (19%) ACE-1 inhibitors and 1 (4.7%) (Table 1).
CKD patients on haemodialysis, admitted for SARS-CoV-2 infection.
| Characteristics | Total | Survivors | Deceased | P-value |
|---|---|---|---|---|
| Female/male | 9/12 | 7/8 | 2/4 | .577 |
| Age | 75.6 | 74.4 | 78.6 | .659 |
| [0,1–5]Comorbidities | ||||
| Arterial hypertension, n (%) | 21 (100) | 15 (100) | 6 (100) | 1 |
| Diabetes mellitus, n (%) | 15 (71.4) | 12 (80) | 3 (50) | .169 |
| Obesity, n (%) | 9 (42.8) | 6 (40) | 3 (50) | .676 |
| Lung disease, n (%) | 10 (47.6) | 5 (33.3) | 5 (83.3) | .038a |
| Ischaemic heart disease, n (%) | 6 (28.5) | 3 (20) | 3 (50) | .169 |
| Stroke, n (%) | 4 (19) | 2 (13.3) | 2 (33.3) | .292 |
| Peripheral vascular disease, n (%) | 6 (28.5) | 5 (33.3) | 1 (16.6) | .445 |
| Active neoplasia, n (%) | 2 (9.5) | 1 (6.60) | 1 (16.6) | .747 |
| ACE inhibitor, n (%) | 1 (4.7) | 1 (6.6) | 0 | .517 |
| ARB, n (%) | 4 (19) | 4 (26.6) | 0 | .16 |
| Calcium channel blockers, n (%) | 7 (33.3) | 6 (40) | 1 (16.6) | .376 |
ARB: angiotensin II receptor blockers; CKD: chronic kidney disease; ACE inhibitor: angiotensin-converting enzyme inhibitor.
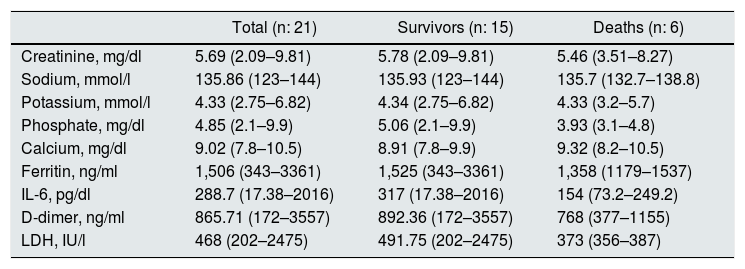
All patients presented with some clinical manifestation, the most frequent was fever together with respiratory symptoms, and both were present in 87% of the cases, while 17 patients (80%) presented with pneumonia by Xray, which was bilateral in all of them. The laboratory variables on admission are shown in Table 2.
Laboratory variables at hospital admission.
| Total (n: 21) | Survivors (n: 15) | Deaths (n: 6) | |
|---|---|---|---|
| Creatinine, mg/dl | 5.69 (2.09–9.81) | 5.78 (2.09–9.81) | 5.46 (3.51–8.27) |
| Sodium, mmol/l | 135.86 (123–144) | 135.93 (123–144) | 135.7 (132.7–138.8) |
| Potassium, mmol/l | 4.33 (2.75–6.82) | 4.34 (2.75–6.82) | 4.33 (3.2–5.7) |
| Phosphate, mg/dl | 4.85 (2.1–9.9) | 5.06 (2.1–9.9) | 3.93 (3.1–4.8) |
| Calcium, mg/dl | 9.02 (7.8–10.5) | 8.91 (7.8–9.9) | 9.32 (8.2–10.5) |
| Ferritin, ng/ml | 1,506 (343–3361) | 1,525 (343–3361) | 1,358 (1179–1537) |
| IL-6, pg/dl | 288.7 (17.38–2016) | 317 (17.38–2016) | 154 (73.2–249.2) |
| D-dimer, ng/ml | 865.71 (172–3557) | 892.36 (172–3557) | 768 (377–1155) |
| LDH, IU/l | 468 (202–2475) | 491.75 (202–2475) | 373 (356–387) |
IL-6: interleukin-6; LDH: lactate dehydrogenase.
The treatment received was hydroxychloroquine in 17 patients (80.9%), azithromycin in 15 (71.4%), lopinavir/ritonavir in 5 (23.8%), ceftriaxone in 4 (19%), darunavir/cobicistat in 2 (9.5%), corticosteroids in one (4.7%) and tocilizumab in one (4.7%).
In the follow-up of the cases, one patient was admitted to the intensive care unit requiring invasive mechanical ventilation (without prone positioning) and the use of vasoactive drugs. Sixteen patients (76%) did not meet the criteria for admission to the ICU during the pandemic period. Six patients (28.5%) died. The presence of previous lung disease was associated with mortality in 83.3% (P = .038). There were no statistically significant differences in relation to the laboratory variables or the treatment received.
Due to the need for isolation to perform the haemodialysis session in patients affected by SARS-CoV-2 infection, PCR was performed routinely every seven days approximately, and after the first negative result it was confirmed after 48 h according to protocol and then the isolation of the patient was discontinued. The mean time to negativisation was 22 days in the studied group. Two patients did not negativise the PCR during their hospitalisation.
The mortality of CKD patients on haemodialysis infected with SARS-CoV-2 was 28.5% and was associated with the presence of previous lung disease. Our results are in concordance with other previously published studies.1–5
The high lethality of the infection in this population group is striking, and could be related to characteristics such as age, close contact with health personnel, in addition to the comorbidities present in this patient profile such as vasculopathy (in the form of ischaemic heart disease, cerebrovascular disease and peripheral arterial disease), as well as diabetes and lung diseases, already described in previous studies.6 In our cohort, it was associated with a history of lung disease.
The mean time to negativisation of the SARS-CoV-2 PCR of naso-oropharyngeal swab was 22 days and remained positive in two patients. Previous studies have shown that the persistence of positive PCR in respiratory samples was associated with greater severity, being 21 days in patients with severe symptoms and 14 days in cases of moderate disease.7,8
It is interesting to mention that the correlation between positive SARS-CoV-2 PCR and infectivity is not clear after the remission of the symptoms; so cases where persistently positive by PCR and did not mean that persisted in an infective state.9 The same occurs in the cases of re-positivisation of SARS-CoV-2 PCR.10
We may conclude that SARS-CoV-2 infection in CKD patients on haemodialysis has an elevated mortality rate, since one out of four hospitalised patients dies, although previous lung disease was associated with mortality. More studies are needed to define the appropriate timing to suspend isolation in patients with persistently positive PCR, which is of vital importance in the case of CKD patients receiving haemodialysis, since isolation requires a suitable centre, trained personnel, materials and transport arrangements, as well as concern for the family environment. The use of SARS-CoV-2 serologies offers a more clear picture of the temporality of the infection, as well as safety when ending the isolation of some patients.
Conflicts of interestMaría José Soler declares that she has conducted scientific consulting work or given presentations for Mundipharma, Fresenius, Bayer, Novo Nordisk, Janssen, Boehringer, Eli Lilly, AstraZeneca and Esteve, not related to this study.
Clara García-Carro declares that she has conducted scientific consulting work, given scientific presentations and/or provided logistical support in organising scientific events for Astra Zeneca, Novo Nordisk, Boehringer Ingelheim, Astellas, Menarini, Novartis, Esteve and Sanofi, not related in any way to this study.
José Zúñiga, Néstor Toapanta, Natalia Ramos, Sonia Caparros, Juan León-Roman, María Azancot and Daniel Serón declare that they have no conflicts of interest.
Please cite this article as: Zúñiga J, Toapanta N, Ramos N, Caparros S, León-Roman J, Azancot M, et al. Infección por SARS-CoV-2 en pacientes con enfermedad renal crónica en hemodiálisis. Evolución de la PCR de SARS-CoV-2. Nefrologia. 2021;41:476–478.