Malignancy is detected three times more in kidney transplant (KT) recipients than general population. Posttransplant lymphoproliferative disorders (PTLD) constitute nearly 20% of malignancies diagnosed after solid organ transplantations. Even though Hodgkin lymphomas (HL) formerly defined as Hodgkin Disease are less common lymphomas after transplantation compared to general population (HL accounts 13% and 7% of lymphomas in general population and posttransplant recipients respectively), relative risk for HL is 2.6 among posttransplant patients compared to the risk among kidney disease patients on waiting list. The incidence of HL after kidney transplantation was approximately reported as 0.1%.1 The average age at diagnosis of posttransplant HL was found as 48.6±11.9 years with male predominance (55% of the cases).
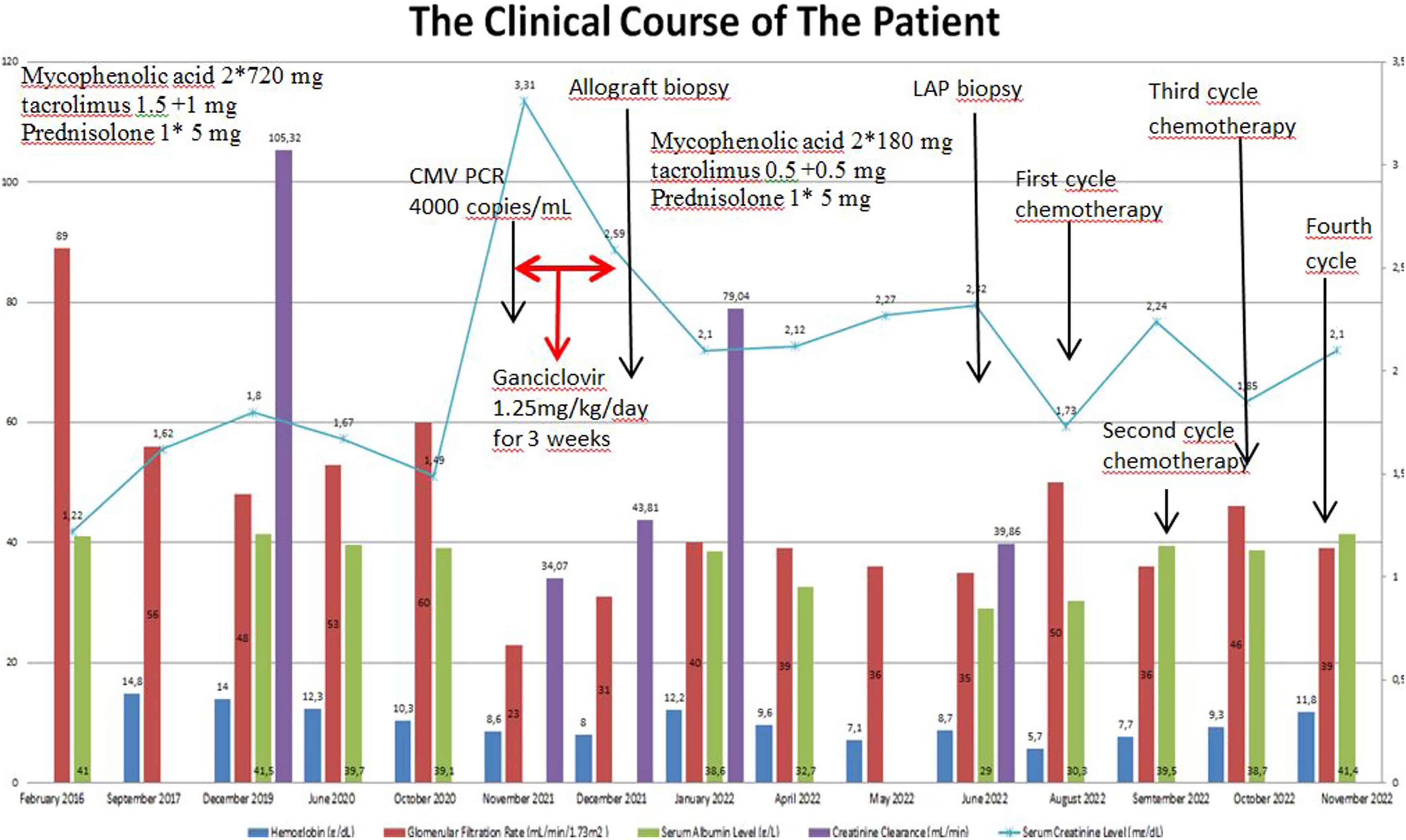
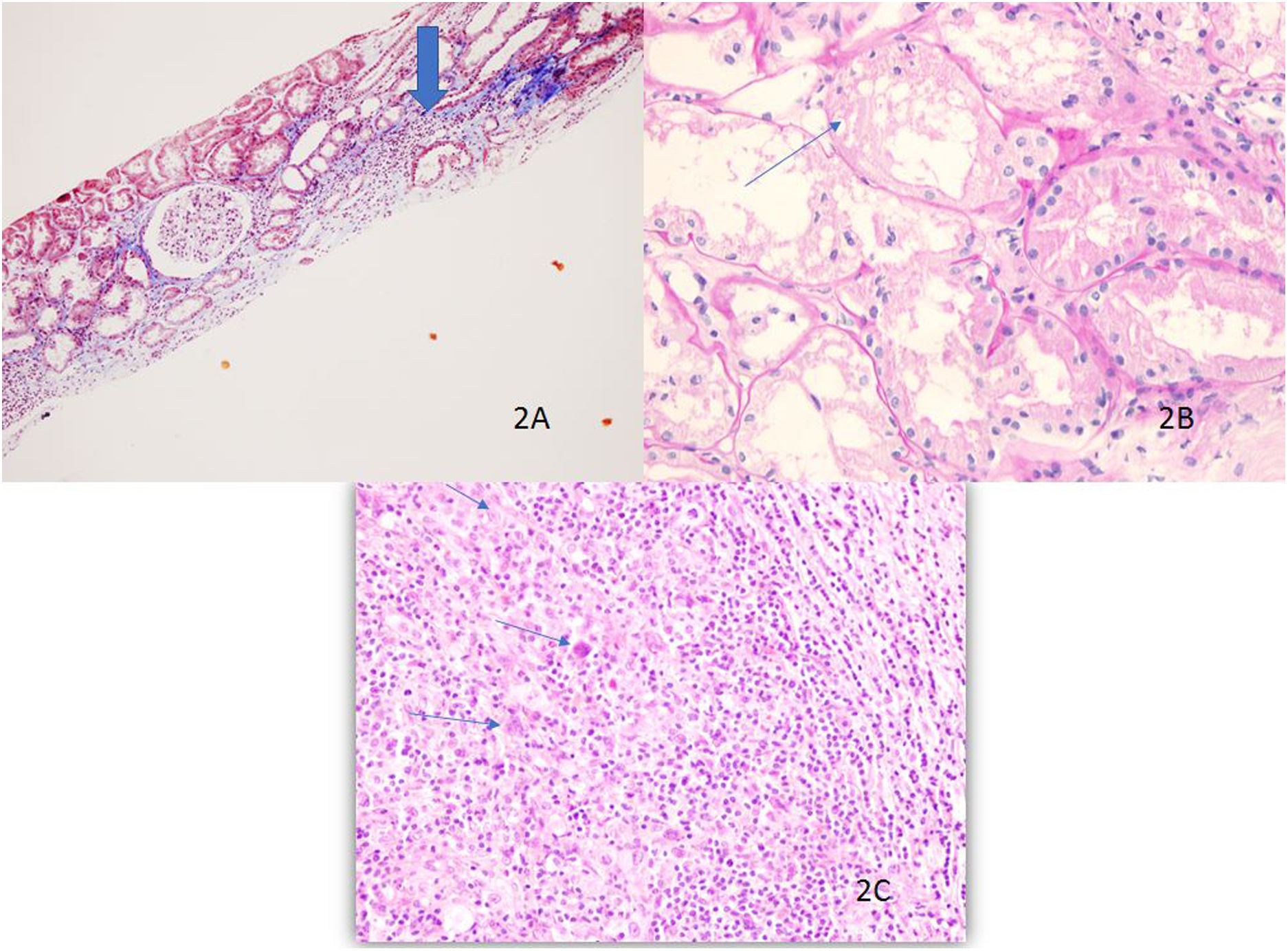
A 35-year-old male patient had a history of kidney transplantation due to chronic kidney failure with unknown etiology 11 years ago in another center. He had COVID-19 infection two years ago. In addition, he was diagnosed with cytomegalovirus (CMV) disease eight months ago during evaluation for acute elevation in serum creatinine levels to 3.3mg/dL and treated via i.v. ganciclovir by then (Fig. 1). The doses of tacrolimus and mycophenolic acid were also decreased. Kidney biopsy revealed chronic allograft nephropathy (Fig. 2). While these infections the patient had night sweats, fever, and weight loss. Splenomegaly was discovered by abdominal ultrasonography coincidentally. While exploring severe anemia (hemoglobin level: 5.7g/dL), multiple lymphadenopathies (LAP) approximately 3cm in size were detected by computed tomography. The patient had been diagnosed with nodular sclerosis classic HL (NSCHL) as the laparascopic excisional biopsy of paraaortic LAP resulted in NSCHL (Fig. 2) with atypical cells positive for CD30, weakly positive for PAX5, but negative for PanCK, CD45, CD20, CD3, CD15, CD79a.
Allograft biopsy shows interstitial fibrosis, tubular atrophy and an area of inflammation (thick arrow) by light microscopy, masson trichrom ×40 (A), the presence of desquamation and necrosis in the tubule epithelium is shown (thin arrow) PAS ×400 (B), Hodgkin cells in the lymphoid background are indicated by arrows, H&E ×400 (C).
Our case had negative blood serology for EBV (monospot test for heterophile antibodies was not reactive) but Epstein-Barr Virus (EBV)-encoded small RNAs (EBER) were positive in lymph node biopsy by in situ hybridization. The patient was evaluated as stage 4 HL based on Ann Arbor staging system as the positron emission tomography (PET) revealed hepatic, splenic and vertebral involvement in addition to multiple LAP on both sides of diaphragm. Afterwards, tacrolimus dose was decreased and mycophenolate mofetil was ceased and the patient received three cycles of BV+AVD regime: doxorubicine (25mg/m2), vinblastine (6mg/m2), dacarbazine (375mg/m2), and brentuximab (1.2mg/kg). The control PET showed regression of the involvements. Kidney functions and hematological parameters were stable with serum creatinine level of 2.1mg/dL and hemoglobin level of 11.7g/dL. The above treatment regimen was planned to be completed to six cycles.
Generally, the incidence of post-transplant malignancy (PTM) was reported as 6% and this cancer risk for patients with KT was found to be 2–3 times more than general population.1 Even though the most common malignancies diagnosed after solid organ transplantations were known as Kaposi sarcoma, nonmelanomatous skin cancer (NMSC), and non-Hodgkin lymphoma (NHL), the incidence of these cancers after KT differ among countries such as lip cancer with the highest incidence in Austria, Canada, UK, USA, NMSC in Finland and Sweden, and NHL in China.1 The incidence of HL was reported as 0.1% in the study conducted among 66,159 kidney transplant recipients between 1991 and 2000 in the United States. The risk ratio for HL in KT recipients was reported as 1.4 by univariate analysis and 2.7 by multivariable analysis. Still, the reported adult HL cases after KT are very few being less than 10, as far as we know.2
Although, calcineurin inhibitors (CNI) are well-known risk factors for the development of lymphoma after KT and reduction in immunosuppression (RIS) is needed in KT patients after the development of lymphoma, absence of CNI is an independent risk factor for allograft loss of these patients by leading to acute rejection. Instead of total cessation of CNI, decreased doses aiming for half of the trough levels (1.5–3.5ng/mL) with continuing steroids and permanent interruption of antimetabolites are recommended. We applied this regimen to our patient and his graft function has been stable without acute rejection episode.
In conclusion, we would like to emphasize the importance of targeting the appropriate CNI trough levels in KT patients, the awareness of carcinogenesis ten years after KT, searching for the appearance of lymphadenopathies and splenomegaly, reminding HL risk (although very rare) among KT recipients, and preserving the graft functions without acute rejection and HL progression.
Ethics approval and consent to participateWritten informed consent was obtained from patient.
Informed consentInformed consent was obtained from the patient.
Compliance with ethical standardsAuthors have no conflicts of interest. No fund was taken.