Fibrillary glomerulonephritis (FGN) is a glomerular disease with organized deposits of immunoglobulins, negative Congo red staining and 16−24 nm fibrils visible in electron microscopy (EM). The clinical syndrome in these patients is variable: nephritic or nephrotic syndrome, microhematuria, hypertension, renal failure and, rarely, rapidly progressive glomerulonephritis (RPG), pulmonary hemorrhage or thrombotic microangiopathy (TMA).1–6 We describe a FGN, with RPG, pulmonary hemorrhage, and positive ANCAp and TMA.
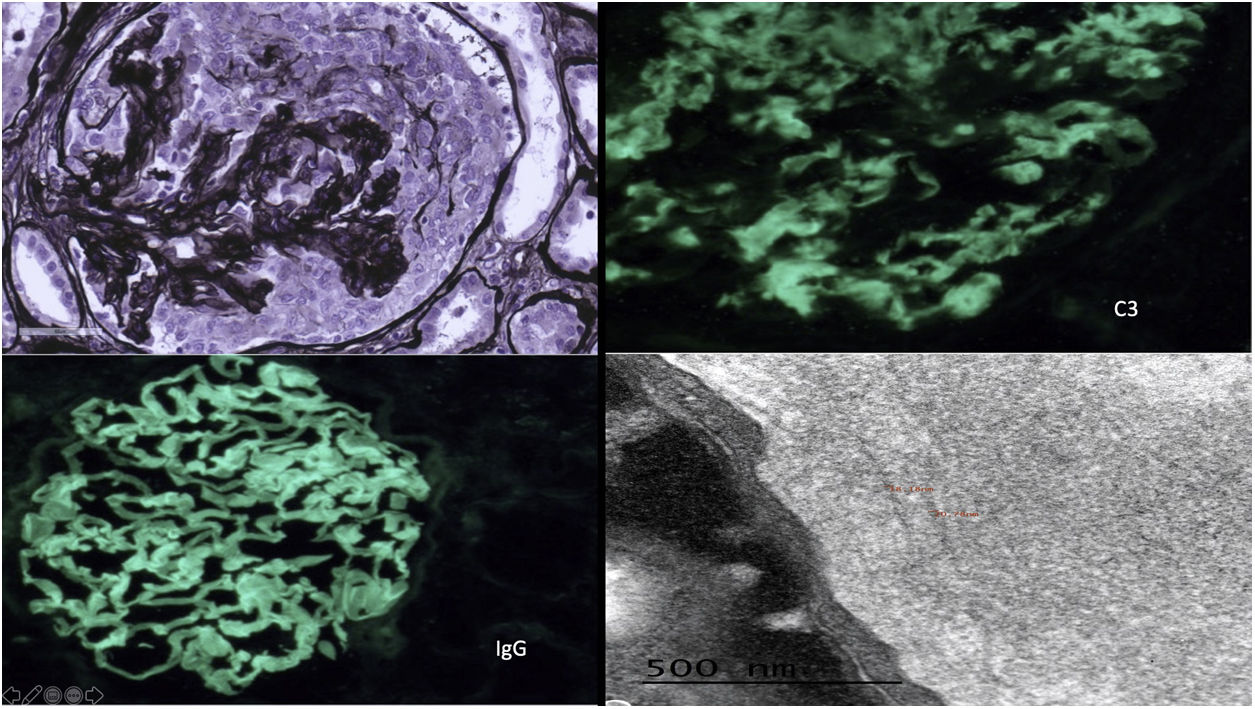
Female, 51 years old, with no relevant medical history, consults for dyspnea and edema. On examination, blood pressure 170/100 mmHg, sinus rhythm, crackles in both lung bases and edema. Hemogram and blood chemistry: normocytic normochromic anemia, without microangiopathic hemolytic anemia (MHA), creatinine 6 mg/dl, nephrotic proteinuria with normal serum albumin and microhematuria. Chest X-ray: bilateral interstitial infiltrate, with diagnosis of pulmonary hemorrhage with immunological study with ANCAp positive 1/320, rest normal/negative, including anti-glomerular basement membrane antibodies. Plasmapheresis, corticosteroids and intravenous cyclophosphamide were started. One week after admission, MHA with smear showing schistocytes and undetectable haptoglobin, with negative stool culture, normal ADAMTS13, we decided to start eculizumab treatment, with normal genetic follow-up Renal biopsy: 49 glomeruli, 10 sclerosed, 29 with epithelial crescents, some with segmental necrosis, PAS and Jones silver positive. No signs of TMA. Direct immunofluorescence was strongly positive for IgG with linear pattern, kappa and lambda positive, weak C3 with parietal and mesangial granular pattern, IgG4 positive (Fig. 1).
Upper left: glomerulus with circumferential epithelial crescent with disruption of the basement membrane and positive staining of the basals and mesangium. Jones silver ×40. Upper right: mesangial granular and pseudolinear 2+ de C3 positivity. IFD C3 × 40. Lower left: linear/pseudolinear 3+ parietal IgG positivity. IFD IgG × 40. Lower right: by EM, dense, banded and continuous deposits, linear in appearance, are observed along the lamina densa of the glomerular basement membranes and in the mesangium constituted by randomly arranged fibrils, whose mean thickness was 18.41 nm.
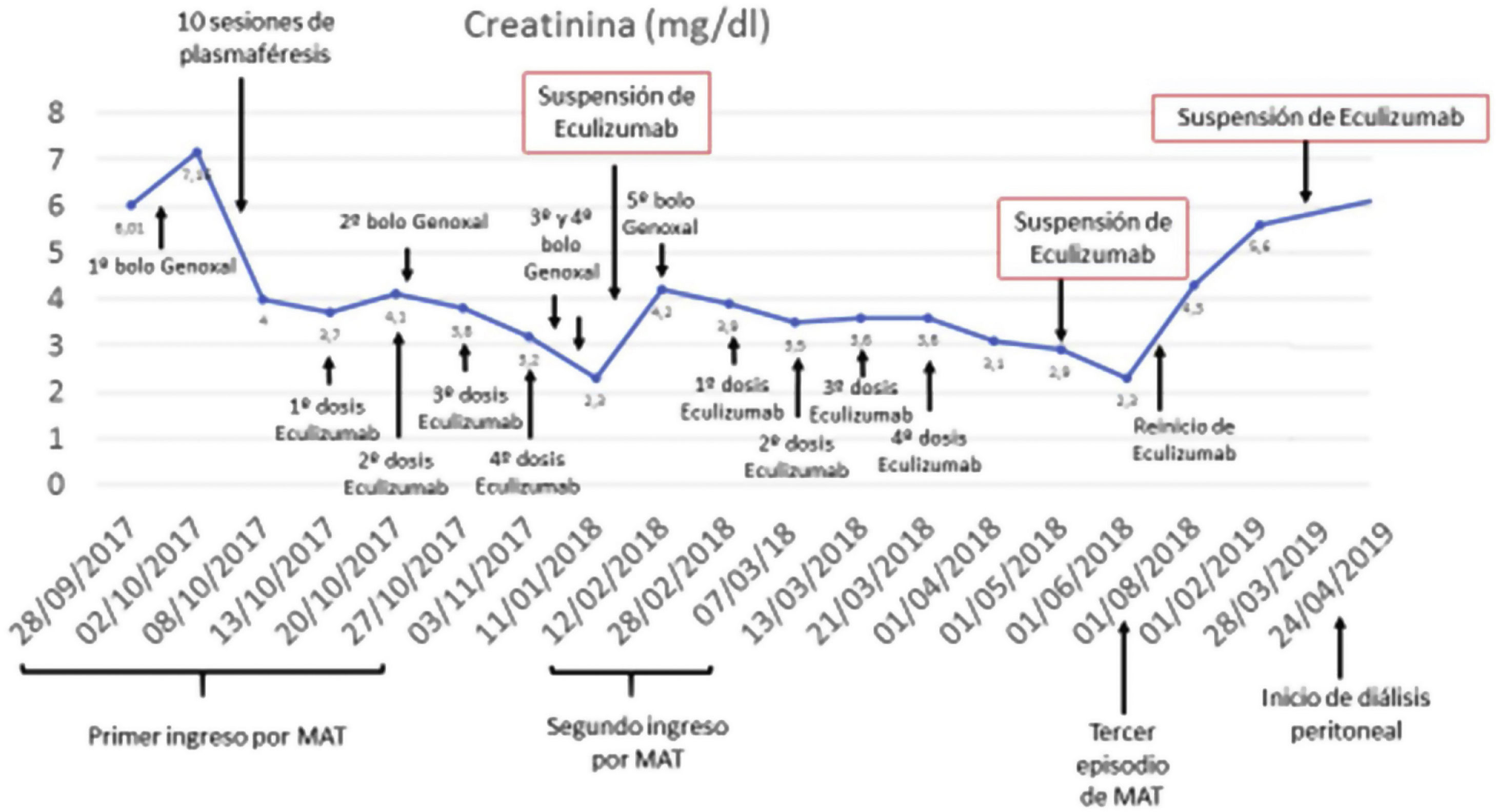
At hospital discharge, the patient presented remission of pulmonary hemorrhage and resolution of MHA, creatinine of 3.8 mg/dl, proteinuria and microhematuria, and continued treatment with cyclophosphamide, corticosteroids and eculizumab up to 2 months after resolution of MHA. Thirty days after discontinuation of eculizumab, she presented a new episode of probable TMA and the ME result was received: dense deposits, in glomerular basement membrane (GBM) and mesangium, consisting of random fibrils, with an average thickness of 18.41 nm, compatible with fibrillary glomerulopathy, with linear IgG deposits (Fig. 1). DNAJB9 testing by immunohistochemistry was positive, and we restarted eculizumab, with suspicion of secondary TMA. After 6 months of cyclophosphamide, we maintained treatment with azathioprine. For 2.5 months, she presented clinical and renal function stability, with no MHA data; treatment with eculizumab was maintained for 3 months and subsequently renal function improved with no MHA data. Three months after discontinuation, the patient presented deterioration of renal function, and eculizumab was reinitiated until her inclusion in chronic treatment with peritoneal dialysis, 9 months later (Fig. 2).
Fibrillary glomerulonephritis rarely presents as it did in this case, with acute renal failure and pulmonary hemorrhage. Different authors suggest the possibility of a circulating factor in GF, which may be responsible for the existence of fibrillar material at pulmonary level, triggering pulmonary hemorrhage.5 For the diagnosis of FGN, EM is necessary, or DNAJB9 by immunohistochemistry if EM is not available. In our case, despite diagnosis made by EM, we tested for DNAJB9 with a positive result.7–9 The linear/pseudolinear IgG deposits described in FGN and in our patient resembles a GBM antibody disease, which makes us rule out FGN when present or suggest coexistence.1,2 The presence of RPG and TMA is rare, but may occur in FGN, even in association with GBMD.1,2,4,7 In fact, Bircan et al. explain that the concurrence of these entities may be due to endothelial injury produced by vasculitis in patients with susceptibility due to FGN with factor H deficiency, triggering TMA in patient with vasculitis and FGN. In our patient we ruled out susceptibility due to absence of factor H deficiency, but the 3 conditions coexisted: FGN, vasculitis, and TMA.10 FGN probably associated with GBMD with ANCAp+ and TMA has not been previously described in the literature, to our knowledge.