We present the case of a 53-year-old man on long-term hemodialysis since July 2008 secondary to diabetic nephropathy. His previous medical history included type 2 diabetes with poor metabolic control, morbid obesity, hypertension (HTN), severe mixed dyslipidaemia, secondary hyperparathyroidism, hyperuricaemia and Child-Pugh B7 chronic alcoholic liver disease. In August 2016, he developed erosive, vesicular, painful lesions on his upper limbs, abdomen and lower limbs which became worse when exposed to the sun. Tests for faecal protoporphyrins were positive (53μg/g) and skin biopsy was compatible with the diagnosis of porphyria cutanea tarda (PCT). The patient began joint follow-up with dermatology. However, his lesions became worse (especially on his upper limbs) and were associated with severe joint pain. In July 2017, it was decided to start treatment with chloroquine, with improvement of the lesions and pain until he became asymptomatic.
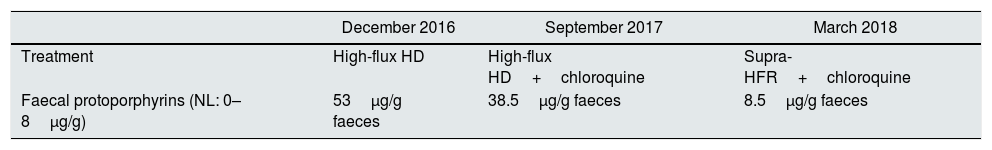
After three months of treatment without modifying his life habits or his usual treatment, he had a new flare-up of very painful skin lesions associated with arthralgia and limited mobility in the interphalangeal joints of both hands (Figs. 1–4). After consultation with dermatology, it was decided to change conventional high-flux hemodialysis to haemodiafiltration with ultrafiltrate regeneration by resin adsorption (Supra-HFR), with clear improvement of skin lesions after three sessions and virtual resolution of the lesions and pain after two weeks of treatment. Protoporphyrins were again determined after three months on this technique to confirm clinical-biological correspondence, with clear improvement with respect to previous determinations, as shown in Table 1.
Changes in laboratory results according to treatment.
| December 2016 | September 2017 | March 2018 | |
|---|---|---|---|
| Treatment | High-flux HD | High-flux HD+chloroquine | Supra-HFR+chloroquine |
| Faecal protoporphyrins (NL: 0–8μg/g) | 53μg/g faeces | 38.5μg/g faeces | 8.5μg/g faeces |
HD: hemodialysis; NL: normal limits; Supra-HFR: haemodiafiltration with ultrafiltrate regeneration by adsorption in resin.
Porphyrias are a group of metabolic diseases caused by deficiencies in the enzymes involved in the metabolism of the haem group, usually due to a genetic mutation. PCT is the most common in Spain and, as its name suggests, it usually manifests with late-onset skin lesions. This type of porphyria is caused by an acquired inhibition of the activity of the enzyme uroporphyrinogen decarboxylase (UROD) in the liver secondary to heterozygous genetic mutations which predispose to the development of the disease. Other factors such as iron treatment, alcohol consumption and tobacco use, hepatitis C virus or HIV infections, or oestrogen consumption can trigger or worsen the condition.
Supra-HFR is an extrarenal purification technique that combines convention, adsorption and diffusion. It has been used with good results in multiple myeloma,1 in the control of inflammatory markers due to a decrease in proinflammatory cytokines (NOS, IL-6 and p-Cresol),2–4 and has even been used for the control of intradialytic HTN5 and nevirapine poisoning in the treatment of HIV.6
Our case is the first to describe a possible role of the Supra-HFR technique in the treatment of metabolic diseases such as PCT. Clinical trials are needed to confirm this effect plus experimental studies to determine the mechanism by which it is produced. One hypothesis would be that this technique could remove the inflammatory molecules deriving from oxidative stress secondary to the overproduction and accumulation of porphyrins, with the consequent improvement of the patient's symptoms.
Please cite this article as: Monzón T, Parodis Y, Valga F, Henríquez F, Antón Pérez G. Uso de HFR-supra para el tratamiento de porfiria cutánea tarda en paciente en hemodiálisis crónica. Nefrologia. 2019;39:216–218.