Patients with chronic kidney disease in the hemodialysis program are exposed to large amounts of water, as this constitutes about 96% of the dialysis fluid. It is known that the use of better quality water decreases the state of chronic inflammation in dialysis patients. Disinfection as part of water treatment plays an important role in meeting the established quality standards; currently, heat disinfection is highly recommended, however the dose of it is not clearly established in the literature. The objective of this review is to know what is available in the literature on the dose of heat disinfection that should be used in hemodialysis and to present our experience with this method at a set dose of 12.000 A0.
Los pacientes con enfermedad renal crónica en programa de hemodiálisis se encuentran expuestos a grandes cantidades de agua ya que este constituye cerca del 96% del líquido de diálisis. Es conocido que el uso de agua de mejor calidad disminuye el estado de inflamación crónica en los pacientes en diálisis. La desinfección como parte del tratamiento del agua tiene un papel importante para cumplir los estándares de calidad establecidos; actualmente la desinfección por calor es altamente recomendable, sin embargo, la dosis de la misma no está claramente establecida en la literatura. El objetivo de esta revisión es conocer lo disponible en la literatura sobre la dosis de desinfección por calor que se debe utilizar en hemodiálisis, así como presentar nuestra experiencia con este método a una dosis establecida de 12.000 A0.
Chronic kidney disease patients on regular hemodialysis (HD) are exposed to large amounts of water (between 90 and 190 liters per session)1 as it is the main component of the dialysis fluid. The semipermeable dialyzer membrane is the only barrier that separates the dialysis fluid from the patient's blood. The presence of chemical and biological contaminants in the water in contact with the blood has a negative impact in patient's health as clearly documented in previous publications Based on the available evidence, the clinical practice guidelines2,3 establish the quality standards of the water to be used use in hemodialysis sessions to prevent complications associated with dialysis fluid.
The water treatment for use in the HD session includes 3 phases. The first one, is to eliminate most of the suspended particles, the organic substances and reduce the number of cations (decalcifier, carbon filter, sand filter) and this is known as the pretreatment phase. The second phase aims to eliminate traces of chemical compounds and bacterial contaminants (reverse osmosis); this is the treatment phase. And the third phase, known as post-treatment, aims to ensure the distribution of water to the monitors, taking into account that circuit designs with external curvatures or sack bottoms favor water stagnation with the risk of contamination.
The guide of dialysis fluid quality of the Spanish Society of Nephrology (SEN)4 establishes 2-standards of water quality for biological contaminants and defines as purified water the presence of ≤100 colony forming units (CFU) ) per milliliter and ≤0.25 endotoxin units (EU) per milliliter and ultrapure water is defined as the presence of ≤10 CFU/ml and ≤0.03 EU/ml.
When the burden of microbial contamination is high, it may produce serious complications that require urgent action in the patient. If the contamination is low, the clinical expression is less evident but consequences are not less dangerous. Today we have sufficient evidence to state that chronic exposure to a low biological contamination burden causes a state of chronic inflammation of low intensity, which is related to the development of ateromatosis, oxidative stress, malnutrition, anemia, resistance to Erythropoietin and mortality from any cause.1,5,6 For this reason, the new guides for water quality management of dialysis fluid (2016) introduce in their recommendations the regular use of ultrapure liquid in all types of HD to prevent and delay the onset of these complications.4
To ensure the inactivation/elimination of microflora in water, there are moderns
treatment plants that effectively produce water that meets the quality requirements; but, in addition, it is necessary to have adequate disinfection systems that guarantee the maintenance of water quality standards throughout the entire distribution circuit. The effectiveness of disinfection systems will be determined by 2 key aspects:
Frequency of disinfection. The frequency of disinfection of the distribution circuit must follow a strategy for prevention of contamination, and also incorporate a periodic evaluation of results and a modification of the strategy based on the results obtained (validation/revalidation system).
Distribution. The disinfection must reach all the elements of the system: reverse osmosis membrane, distribution circuit system, entrance to the monitors and to the dialysis monitor itself. To guarantee this, it is essential, an adequate design of the distribution circuit that avoids dead zones and sack bottoms.
The germicidal systems available for disinfection have a number of disadvantages. It is known that chlorine infusion at the beginning of pretreatment can alter the characteristics of certain osmosis membranes; submicron filters prevent the passage of bacteria larger than 0.1 µ; Ultraviolet radiation lamps need a good design to be effective, their effect depends on the power of the lamp, the purity of the water, the time and flow of exposure, and its main danger is the massive release of endotoxins in heavily polluted waters; the ozone required for its elimination of a high power multifrequency ultraviolet lamp for its transformation into molecular peroxide; and finally, periodic disinfection of the plant using descaling and disinfectant substances requires the clearance of these substances and subsequent verification of residual level (established for each substance). As for heat disinfection, it is being used currently but without knowing the necessary dose to ensure adequate disinfection.
Concept of disinfectionEtymologically disinfection is a chemical concept that refers to the elimination or inactivation of pathogens found in an inert object. But there is no clear definition for term disinfection since it refers to compliance with a series of quality standards, that apply for a specific context and circumstance8 (for example, the concept of disinfection of a hospital potty is totally different from the concept that we apply to the disinfection of the surgical material or the HD circuit ).
Recently the concept of heat dose has been introduced, understood as the energy needed to eliminate/inactivate certain microorganisms in a given context. That is, a given dose of heat will achieve a given disinfection.9 The objective of this review is to know the data available on the dose of heat disinfection that should be used in HD, as well as present our experience with this method using the dose established.
Heat doseIt is a theoretical concept that expresses the relationship between the temperature applied and the time of exposure required to achieve a defined inactivation of microorganisms. This relationship expresses the energy applied, which is proportional to the temperature and time exposed of the material that we want to disinfect.
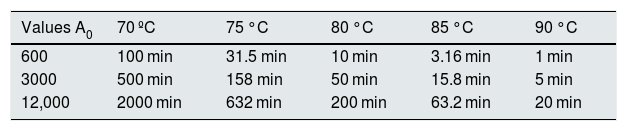
The parameters that govern the dose of thermal disinfection are defined and controlled by the value A0 by EN ISO 15883-1,10 in which a unit of A0 means a second at 80 °C, which causes some disinfection, known as the value of z. This value is a measure in °C of the relationship between the temperature and destruction process by which you can know the increase in temperature required to reduce the D value of a microorganism (the D value is the length of time required, of a given temperature, to eliminate/inactivate 90% of the population of microorganisms). The z value is also used in the concept A0. A value A0 can be achieved with the various combinations of time and temperature (Table 1).7
Exposure times at different temperatures to achieve A 0 values of 600, 3000 or 12,000.
| Values A0 | 70 ºC | 75 °C | 80 °C | 85 °C | 90 °C |
|---|---|---|---|---|---|
| 600 | 100 min | 31.5 min | 10 min | 3.16 min | 1 min |
| 3000 | 500 min | 158 min | 50 min | 15.8 min | 5 min |
| 12,000 | 2000 min | 632 min | 200 min | 63.2 min | 20 min |
Disinfection is the result of the heat dose applied; that is, a certain dose of heat is applied to eliminate/inactivate a number of microorganisms. For example, applying a dose of 3000 A0, a 99.999% of a particular microorganism is inactivated. To avoid decimals, it is commonly expressed in the form of logarithms (log); so we could say, in a simplified manner, that the logarithm represents the number of 9 in the percentage of deactivated microorganisms. Returning to the example, when applying 3000 A 0 it is obatained a 5 log disinfection (99.999%). The higher the log value, the greater the percentage of eliminated/inactivated microorganisms; this is a method to quantify the degree of disinfection being achieved.
ISO 158883-1 establishes an A0 of 60 as the heat dose necessary for the disinfection of medical devices that come into contact with intact skin,10 while ISO 23500 determines an A0 of 600 as the minimum requirement for thermal disinfection of surgical instruments.11 In HD, the dose is not yet established, but the requirements must be much more demanding, since these are large facilities and there is also the possibility of biofilm formation.
A dose of 12,000 A0, can be applied using different combinations of water temperature and time of exposure (Table 1).7 The table shows that temperature and time are equivalent, and how the different combinations achieve doses of 600, 3000 or 12,000 A0, respectively, and how they all produce the same disinfection.
The concept of Ao allows to calculate all possible combinations of time and temperature to achieve a certain degree of disinfection in a more efficient and economical manner, adapted to the needs of each HD Unit. The automatic programming of thermal disinfection based on this concept offers the possibility of increasing the frequency of procedures, thus favoring the eradication of microbiological activity in the dialysis fluid.
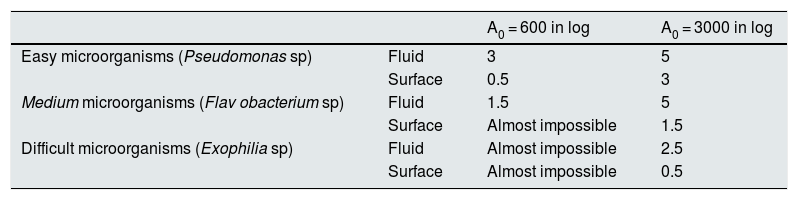
Hemodialysis circuit disinfectionAs explained a given dose of heat (A0 ) applied in a specific context will condition a certain percentage of disinfection. The necessary effective dose will depend on the type of microorganism to be eliminated/inactivated, as well as by the context in which it is applied. Not all microorganisms are equal to eradicate/inactivate (Table 2).7,12
Example of 3 types of microorganisms that are eliminated depending on whether they are in the fluid phase or on the surface (biofilm).
| A0 = 600 in log | A0 = 3000 in log | ||
|---|---|---|---|
| Easy microorganisms (Pseudomonas sp) | Fluid | 3 | 5 |
| Surface | 0.5 | 3 | |
| Medium microorganisms (Flav obacterium sp) | Fluid | 1.5 | 5 |
| Surface | Almost impossible | 1.5 | |
| Difficult microorganisms (Exophilia sp) | Fluid | Almost impossible | 2.5 |
| Surface | Almost impossible | 0.5 |
An important aspect to take into consideration in the HD water plant is that the microorganisms adhered to a surface may be up to 5 times more resistant than if they are in a fluid phase (Table 2), thus elimination is more difficult.13 It is important to take this aspect into account because a detection of small concentrations of microorganisms/endotoxins, in the periodic analyzes performed in our facilities that may be considered acceptable, does not mean the absence of contamination, since this same microorganism could be found as part of a biofilm, which requires higher doses of heat for eradication. Hence it is recommended to maintain an alert proactive attitude to prevent the growth of germs and avoid adhesion to surfaces with formation of biofilm.13
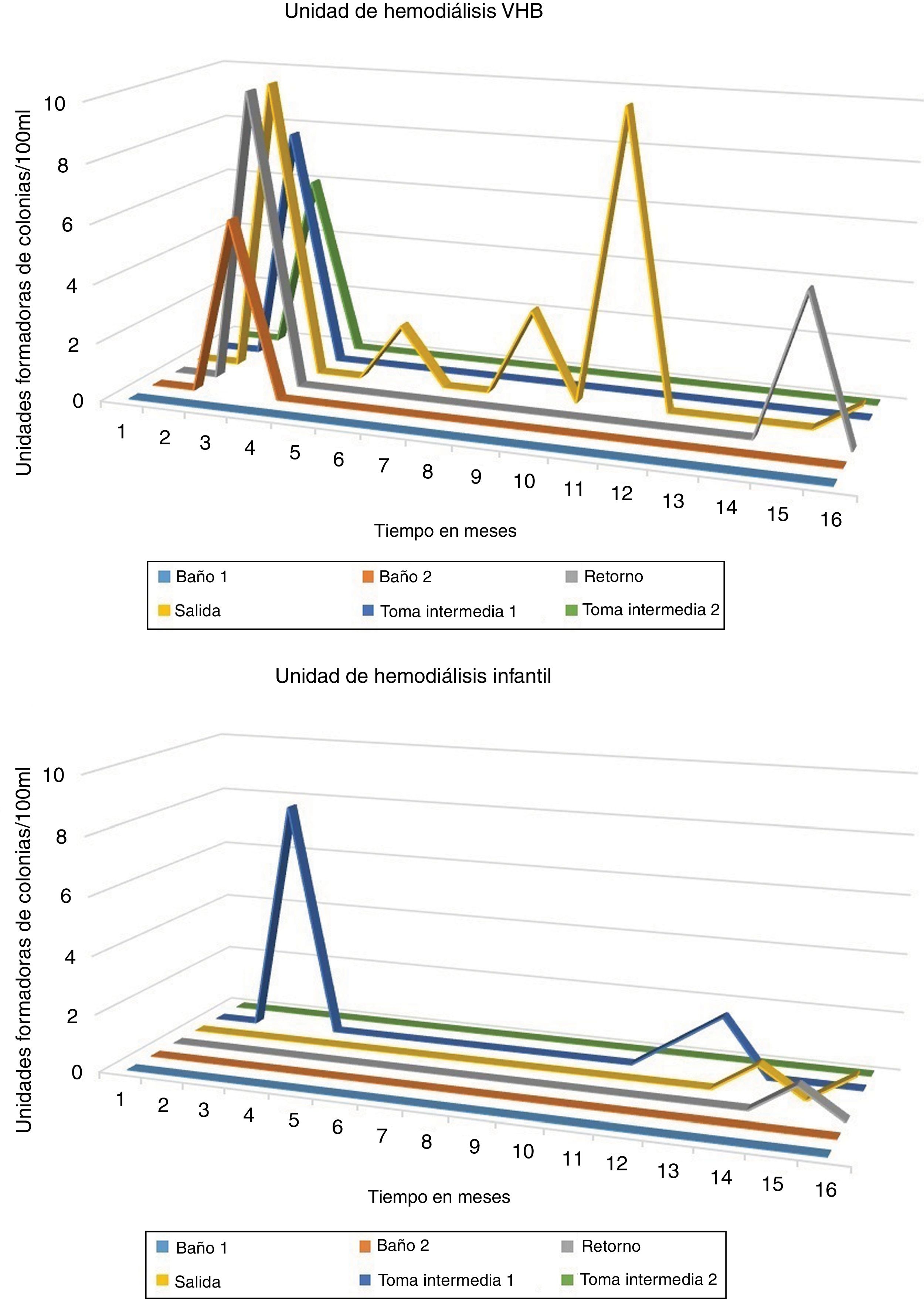
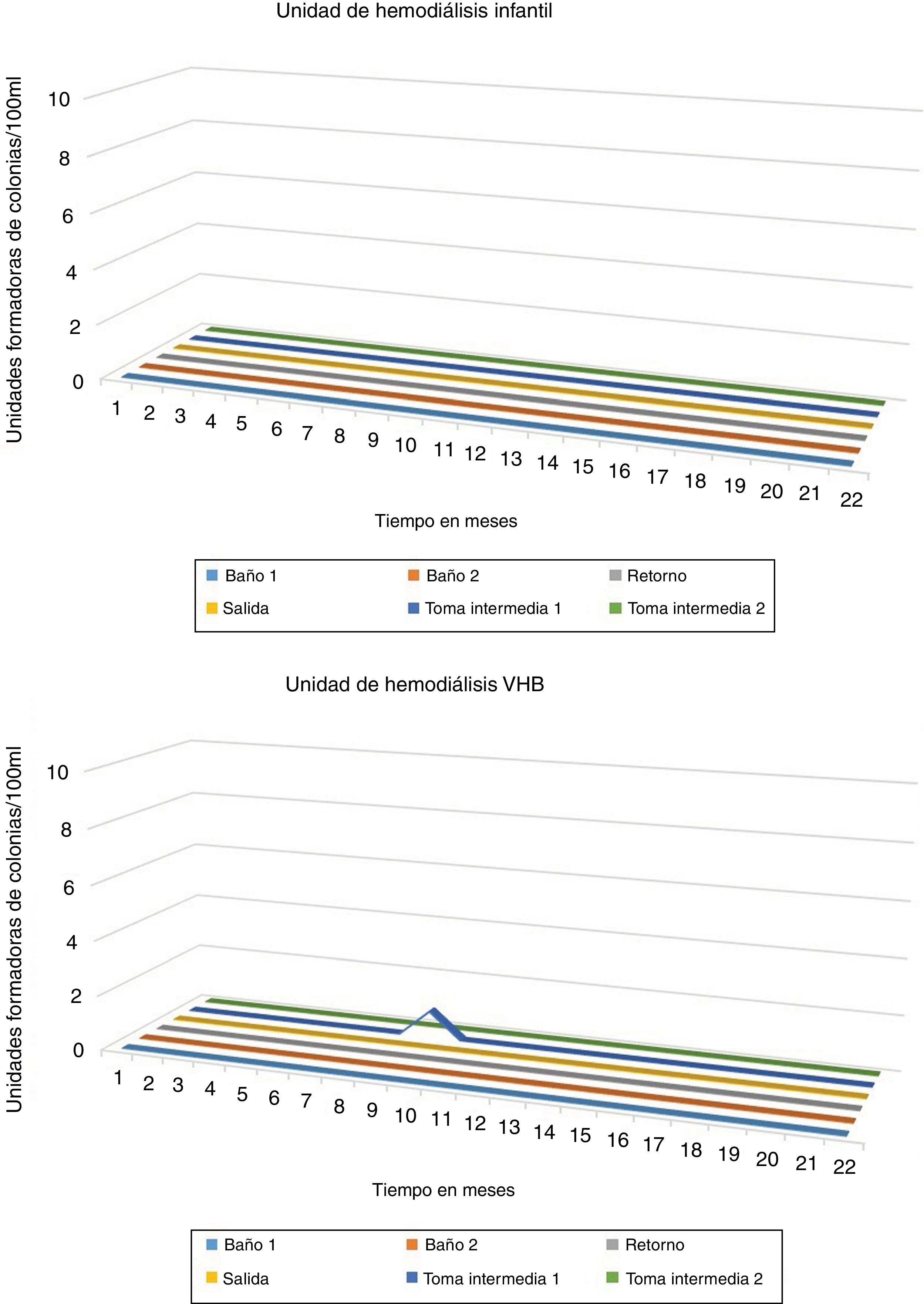
Experience in our centerWe conducted a retrospective observational study in the HD units of the Virgen del Rocío University Hospital, both in the unit of patients infected with hepatitis B virus (HBV) and in the pediatrics HD unit. It was compared the thermal disinfection applied in 2 different periods with different heat disinfection schedules. The HD unit of patients infected with HBV has 12 dialysis stations, with a distance to the water plant of 60 m, while the child HD unit has 5 positions, with a distance to the water plant of 80 m and 2 m high.
In the first period, between January 2013 and May 2014, daily disinfection of the distribution circuit was performed at 65 °C for 120 min and a weekly disinfection at 90 °C (including membranes at 85 °C) for 120 min. In the second period, between June 2014 and March 2016, we used the concept A0 : with 12,000 A 0 daily and applying 90 °C for 120 min to the distribution circuit and membranes. Due to the characteristics of the installation it was necessary to extend this temperature for more time (than the theoretically anticipated) to guarantee that in all points a temperature of 85 °C was maintained for a 60 min period. Moreover, during the second period a safety filter and the (10, 5 and 1 μ) filters were was replaced and in the unit of HBV infected patients three filters (10, 5 and 1 μ ) were also replaced.
Water quality control (microbiological and endotoxins) was performed monthly according to protocol, and samples were obtained from the exit and return to the distribution ciircuit, 2 intermediate samples and monitors. The microbiological analysis was performed by reasoner's 2A agar (R2A) culture during 14 days of incubation at 30–35 °C and endotoxins (Limulus amoebocyte lysates activation, LAL) with reference standards for ultrapure water.4
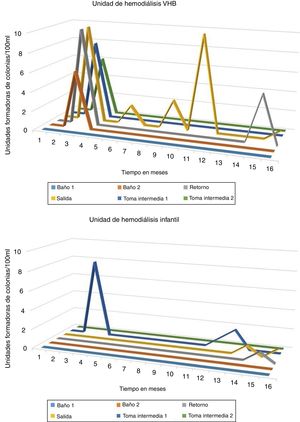
ResultsIn the thermal disinfection carried out between January 2013 and May 2014 (daily disinfection of the circuit at 65 °C for 120 min and a weekly disinfection at 90 °C), growth of CFU was observed in the different samples from both i the HD unit of patients infected with HBV from the children HD unit. The growth of CFU never exceeded the standard for ultrapure water (see Fig. 1).
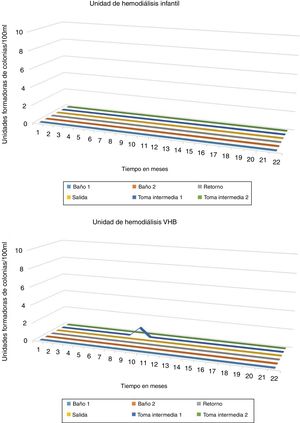
While, in the thermal disinfection carried out between June 2014 and March 2016, using the concept A0, (with 12,000 A0 daily by applying at 90 °C for 120 min in circuit and membranes). Only 1 CFU was observed in the sample of intermediate 1 of the HD unit of patients infected with HBV. Being a single isolated sample, it was likely a contamination. No CFU was detected in the samples corresponding to the HD unit (see Fig. 2).
ConclusionsThese results show the effectiveness of daily heat disinfection. Modern equipment is programmed to start the disinfection process automatically without the intervention of personnel. This allows an integral disinfection that includes both the circuit and the membranes of the osmosis and the monitors. With this procedure, the frequency of the intervention can be easily increased and the development of biofilm in the circuit is avoided, which allows to improve the quality of the water used for dialysis, as shown by our results.
Using the concept of A0 offers the advantage of measuring and programming the dose level applied that can be adjusted to the characteristics of the facilities. Thus, disinfection is efficient and less expensive through combinations between time and temperature, which increase energy consumption. The application of the heat dose of 12,000 A0 results in the elimination of microbiological activity in 2 different HD units.
Key conceptsThe guide of dialysis fluid quality of the Spanish Society of Nephrology recommends the use of ultrapure water in all HD facilities.
Chronic exposure to a low load of biological contaminants causes chronic inflammation that is associated with the development of atheromatosis, oxidative stress, malnutrition, anemia and resistance to erythropoietin.
The effectiveness of disinfection systems will be determined by the frequency of disinfection and distribution. It is essential an adequate design of the distribution circuit to avoids dead zones and sack bottoms in the circuit.
The parameters that govern the thermal dose of disinfection are defined and controlled by the value A0, in which a unit of A0 means a second to 80 °C. A value of A0 value can be achieved with the various combinations of temperature and time.
Using the concept of A0 offers the advantage of measuring and programming the dose applied, achieving a more efficient and economical disinfection by the combinations of time and temperature.
The heat dose of 12,000 A0 is effective in ensuring the disinfection of a water treatment plant and the distribution system of a standard HD unit.
FinancingWe express our thanks to Baxter for supporting the publication of this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Gaibor NGT, Sacaluga LG, Ojeda FdlC, Cotén JRM, Lazo MS. Desinfección térmica en hemodiálisis usando el concepto A0 como dosificador. Nefrologia. 2019;39:482–488.