At the EDTA Congress held in Florence in 1975, Cambi presented the results obtained with a haemodialysis regimen of 3 weekly sessions of 4h duration.1 This report is not the most cited, but it is the one withg greatest impact in the history of haemodialysis. After 40 years have this regimen remains the usual scheme of regular haemodialysis, in both frequency and duration.
Although performing 3 sessions per week is the conventional frequency in most haemodialysis units, an increase in the number of weekly sessions has been generally well-accepted by the nephrological community, and is considered a valid alternative for certain patients. However, a reduction in the weekly frequency of haemodialysis has always been controversial, even a taboo subject in Kalantar-Zadeh's opinion.2 Data from DOPPS 4 show that the frequency of 3 weekly sessions is accepted by the overwhelming majority, and patients who dialyse less often are an anecdotal minority (data referring to Spain indicate that 8% of patients dialyse more than 3 days a week, and only 1% do so less often).3
“Infrequent” haemodialysisIt should be remembered that in 1985 Gotch established that based in the urea kinetic model an adequate dose of dialysis could be achieved with 2 weekly sessions providing that, the residual clearance of urea was equal to or greater than 2.5mL/min.4 Based on the DOPPS study and successive clinical guidelines it seems that this alternative have no many followers. The 2006 KDOQI Guideline evaluated the possibility of starting renal replacement therapy with 2 weekly haemodialysis sessions, when the residual clearance of urea5 was greater than 3mL/min/1.73m.2 But this suggestion was no longer included in the 2015 KDOQI Guideline.6 For years, periodic measurement of renal clearance of urea has not formed part of the follow-up protocol in many haemodialysis units, among other reasons because residual renal function was considered to decline rapidly after commencement of regular HD so its determination had no value. This may be one of the reasons explaining the scant implementation of lower weekly frequency haemodialysis.
Having in mind this background, it is interesting to see the increasing number of publications during the last 4 years, that show results obtained using less that 3 weekly HD sessions.3,7–18 These articles have resulted in the publication of editorials, opinion articles and reviews which reveal real controversies19–24 in the field.
The experiences described in these publications should be classified into 2 groups that are totally different. In some articles, the number of weekly sessions of haemodialysis is adjusted to financial support.3,7,9,11,15,17 Other publications describe the results obtained in patients that started renal replacement therapy with one or two weekly sessions with acceptable residual renal function, and increasing frequency as renal residual function was progressively reduced. This practice, similar to that performed for many years in many peritoneal dialysis units, is called incremental or progressive haemodialysis. To implement this scheme of dialysis it is necessary to have no financial constrain.
Incremental haemodialysisOne aspect highlighted by most of the published experiences is that starting treatment with incremental haemodialysis achieves better preservation of residual renal function.10,12,13,18
Preservation of residual renal function in patient on regular dialysis is important. It allows a greater fluid intake, it contributes to the elimination of medium and large uremic molecules, facilitates anemia correction Reduces inflammation, improves nutritional status, the control of blood pressure and quality of life, and it is a potent predictor of survival.25–27 Therefore the preservation of residual renal function has become one of the goals of haemodialysis treatment.5
As a result of better maintenance of residual renal function, incremental haemodialysis is associated with lower erythropoietin requirements,13,14 better nutritional parameters,9,13 lower concentrations of beta-2-microglobulin,10,13,16 less volume overload according to interdialysis weight gain data,8,9,18 reduced hospitalization requirements,13,14 better parameters quality of life16 and survival rates equal to or greater than those achieved with the usual 3 weekly sessions.9,13,14
It should be taken into consideration that all published work on incremental haemodialysis is observational and all have screening bias. Patients are excluded not only based on the renal function value at the start of haemodialysis treatment, but also if certain comorbidities are present.21,23 The inclusion criteria of the patients may influence the results, and the advantages observed with incremental haemodialysis should be analyzed carefully.
Our 10-year experience with incremental haemodialysisAt the beginning of 2006 we decided to apply incremental dialysis at the commencement of HD therapy. When a patient is admitted to the Haemodialysis Unit, a residual renal function study was performed. Two or three weekly sessions was scheduled depending on whether or not urea clearance exceeded 2.5mL/min.4 Patients that were dialysed twice a week remained with this regimen until residual urea clearance was less than 2.5mL/min or had clinical or laboratory abnormalities which prompted an increased frequency of treatment.
In the initial periods of implementation of this guideline, we excluded cases with a history of heart failure and evidence of volume overload. With time we gained experience and confidence, and these patients have been enrolled in the incremental haemodialysis program; presently the only limiting factor from inclusion is the renal clearance of urea.
Residual renal function, glomerular filtration rate, is measured every 2 months as the mean of 24-h urea and creatinine clearance. The dialysis dose is calculated using the Daugirdas Kt/V, to which the renal clearance of urea contribution is added according to the formula recommended in the 2006 KDOQI guideline.5 This total balanced Kt/V should be equal to or greater than 1.6, which is the minimum value indicated for the regimen of 2 weekly haemodialysis sessions in the Gotch4 and Casino28 nomograms.
Using incremental haemodialysis, we have observed beneficial effects on anemia, beta-2-microglobulin concentration and hospitalization requirements 10,14, without detecting a tendency to volume overload, measured by bioimpedance techniques or by biochemical circulatory volume markers.8,29 The latest version of UpToDate (2016)30 recommends incorporating the measurement of renal function in the calculation of the dialysis dose received by haemodialysis patients, and cites the experience of our group, as we have found that the maintenance of residual renal function is similar between patients who start with 2 sessions of haemodialysis and those who start peritoneal dialysis.10
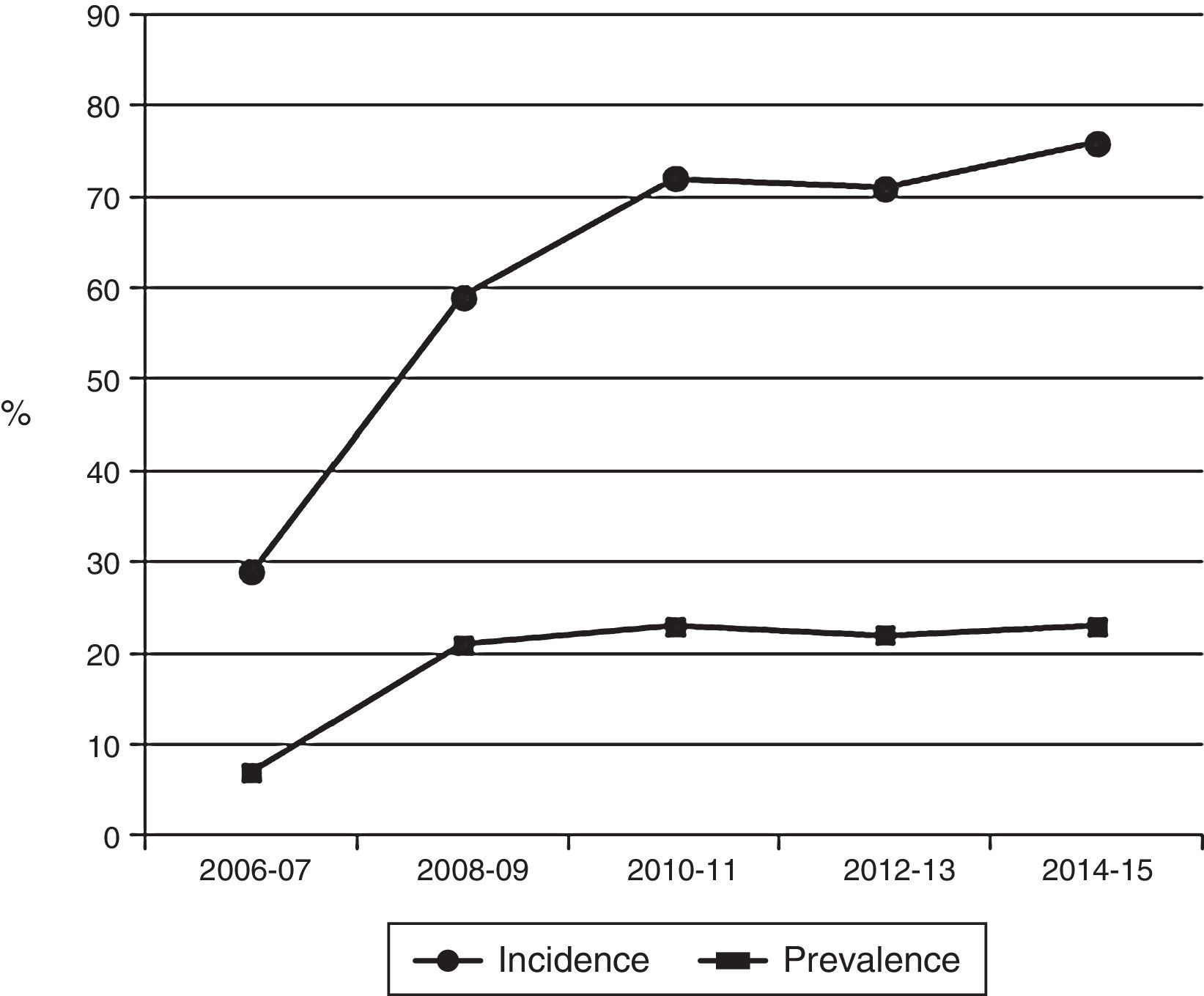
Fig. 1 shows that the percentage of patients who started renal replacement therapy with 2 weekly sessions has increased from 29% to 76%, and that 20–25% of the patients treated in the hospital's haemodialysis unit are continuously being treated at this bi-weekly frequency.
At 24 months after initiation of haemodialysis treatment, 35% of patients treated with incremental haemodialysis maintained a renal function that was sufficient to continue the regime of 2 weekly.14
Our incremental haemodialysis program has been a pioneer in Spain and this experience has been disseminated through various publications.8,10,14,29 We are aware that other haemodialysis units in this country are interested in implementing this type of program and, in this same issue of the journal Nefrología [Nephrology], Merino et al. describe their experience with an incremental regimen similar to ours, and conclude that starting with 2 sessions a week can maintain residual diuresis, at least during the first year of haemodialysis treatment.
ConclusionsStarting renal replacement therapy with 2 haemodialysis sessions per week with presevive increase in the frequency of dialysis session is an innovative clinical practice that changes the practice that has been used for more than 30 years. One of the main goals the preservation of residual renal function in patients who start haemodialysis, with the consequent clinical advantages associated with the maintenance of this renal function.
Our experience, like the rest of the published works on incremental haemodialysis, is an observational study, with the screening bias determined by residual renal function at the commencement of renal replacement therapy. Although this does not invalidate the clinical findings obtained during these 10 years of experience, we believe that it is essential to back up these results with the greatest possible evidence, such as via a multicenter clinical trial that we have already implemented. Demonstrating the efficacy and safety of this regimen through a clinical trial would promote a wider dissemination within the nephrological community.
Please cite this article as: Fernández Lucas M, Teruel JL. Hemodiálisis incremental como forma de inicio del tratamiento sustitutivo renal. Nefrología. 2017;37:1–4.