La warfarina es una causa muy conocida de hematuria macroscópica. Sin embargo, el deterioro de la función renal no ocurre salvo en el caso inusual de gran pérdida de sangre o formación de coágulos que obstruyen el tracto urinario. Recientemente se ha descrito una entidad denominada nefropatía relacionada con la warfarina en la que el fracaso renal agudo es provocado por hemorragia glomerular y obstrucción tubular renal por cilindros de glóbulos rojos. Exponemos el caso de un paciente bajo tratamiento de warfarina con enfermedad renal crónica, hematuria macroscópica e insuficiencia renal aguda. Una biopsia renal mostró una oclusión masiva de túbulos renales por cilindros de glóbulos rojos. Debatimos la posible relación de la terapia con warfarina, la hemorragia intratubular y el fracaso renal agudo.
Warfarin is a well-established cause of gross hematuria. However, impaired kidney function does not occur except in the rare instance of severe blood loss or clot formation that obstructs the urinary tract. It has been recently described an entity called warfarin-related nephropathy, in which acute kidney injury is caused by glomerular hemorrhage and renal tubular obstruction by red blood cell casts. We report a patient under warfarin treatment with chronic kidney disease, macroscopic hematuria and acute kidney injury. A renal biopsy showed massive occlusion of renal tubules by red blood cells and casts. The possible relationship of the warfarin therapy, intratubular hemorrhage and acute kidney injury is discussed.
Background
Warfarin is the most widely used anticoagulant in patients with different disorders to prevent thrombosis. Several adverse effects of warfarin treatment on the kidney have been reported, including acute interstitial nephritis, leucocytoclastic vasculitis, spontaneous cholesterol embolization in patients with diffuse atherosclerosis and ischemic acute tubular necrosis secondary to massive blood loss.1 Recently, it has been suggested that warfarin can also cause acute kidney injury (AKI) in the absence of significant hemodynamic changes, by inducing glomerular hemorrhage and renal tubular obstruction by red blood cell (RBC) casts, a mechanism similar to that observed in IgA nephropathy, crescentic glomerulonephritis and post streptococcal glomerulonephritis.
We hereby report a case of AKI in a patient on warfarin treatment presenting with gross hematuria in the absence of hemodynamically significant blood loss or urinary tract obstruction. Renal biopsy findings helped solving this enigma.
Case report
A 74-year-old-man presented to his community hospital with nose and gum bleeding. Past medical history was relevant for arterial hypertension, pulmonary chronic disease, atrial fibrillation and chronic heart failure class II/IV NYHA. He had chronic kidney disease (CKD), since serum creatinine was 1.8mg/dL three years before admission. He had had myocardial revascularization and biological mitral valve replacement surgery in 2007 complicated by acute stroke. He was on furosemide 120mg daily, cilazapril 5mg daily, carvedilol 6.25 twice daily, eufilin 250mg daily, fluticasone+salmeterol inhalation twice daily, epinitril 5mg transdermal, alopurinol 100mg daily, omeprazol 20mg daily, warfarin and domiciliary oxygen.
On admission, his blood pressure was 110/64mmHg and pulse was 90 beats per minute and he was afebrile. There was no evidence of dehydration. The only abnormal physical finding was wheezing in his lower lung fields. Serum laboratory tests at presentation included an hemoglobin of 8.9g/dL, leukocyte count 14.470/mL with 91% neutrophils, platelet count 375.000/mL, a creatinine of 2.4 mg/dL, urea 185mg/dL and c-reactive protein of 9.88mg/dL. Urinalysis showed proteinuria and hematuria. On admission his international normalized ratio (INR) was 7.0. Radiographic study showed bilateral heterogeneous opacities of the lower lungs. Renal ultrasound showed slightly reduced kidneys with increased parenchyma echogenicity and no hydronephrosis. He was started on ceftriaxone and azithromycin with resolution of lung infection and simultaneously his renal function improved (serum creatinine of 1.9mg/dL). Supratherapeutic INR was corrected with vitamin K and anticoagulation with warfarin was maintained.
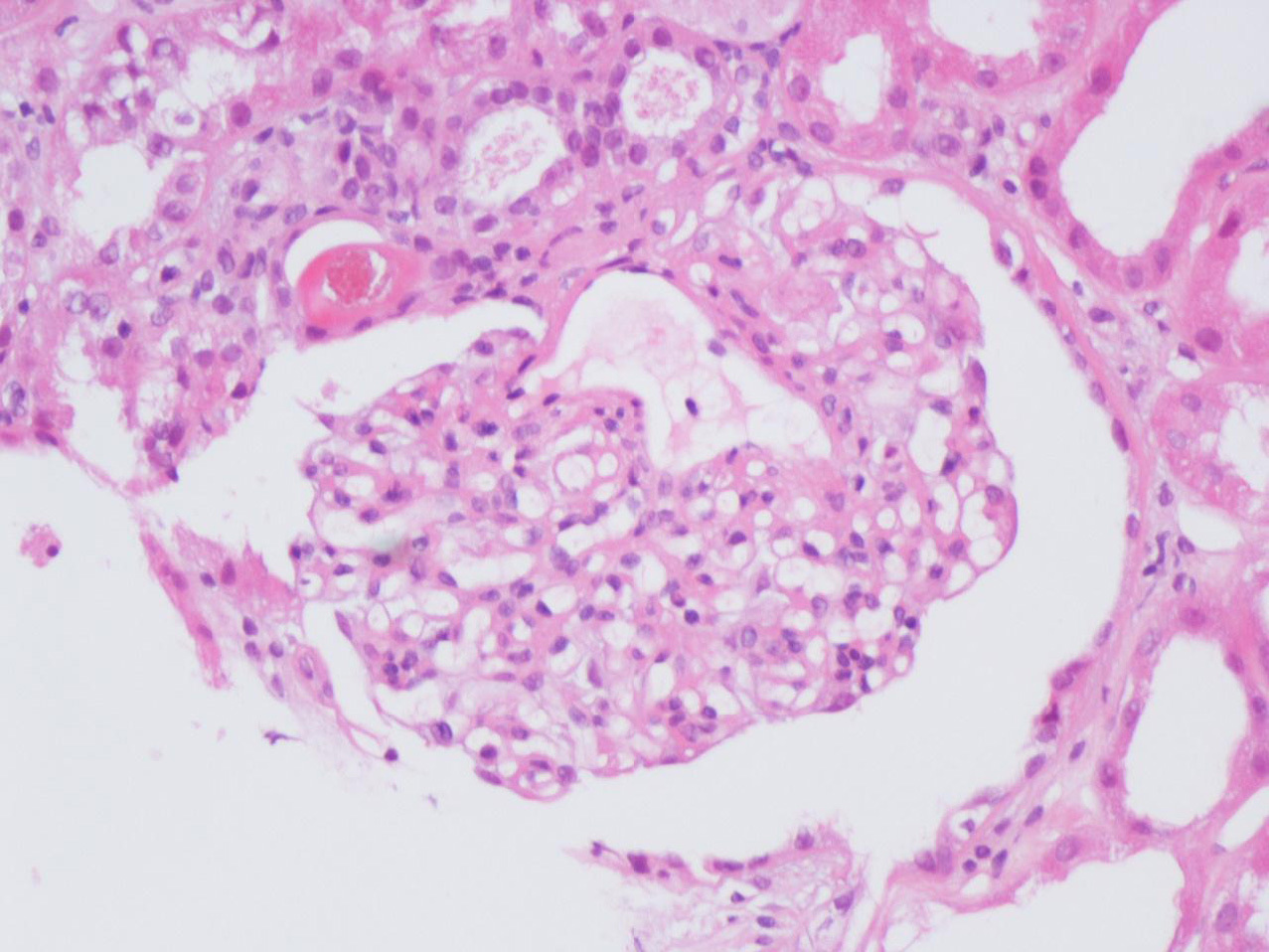
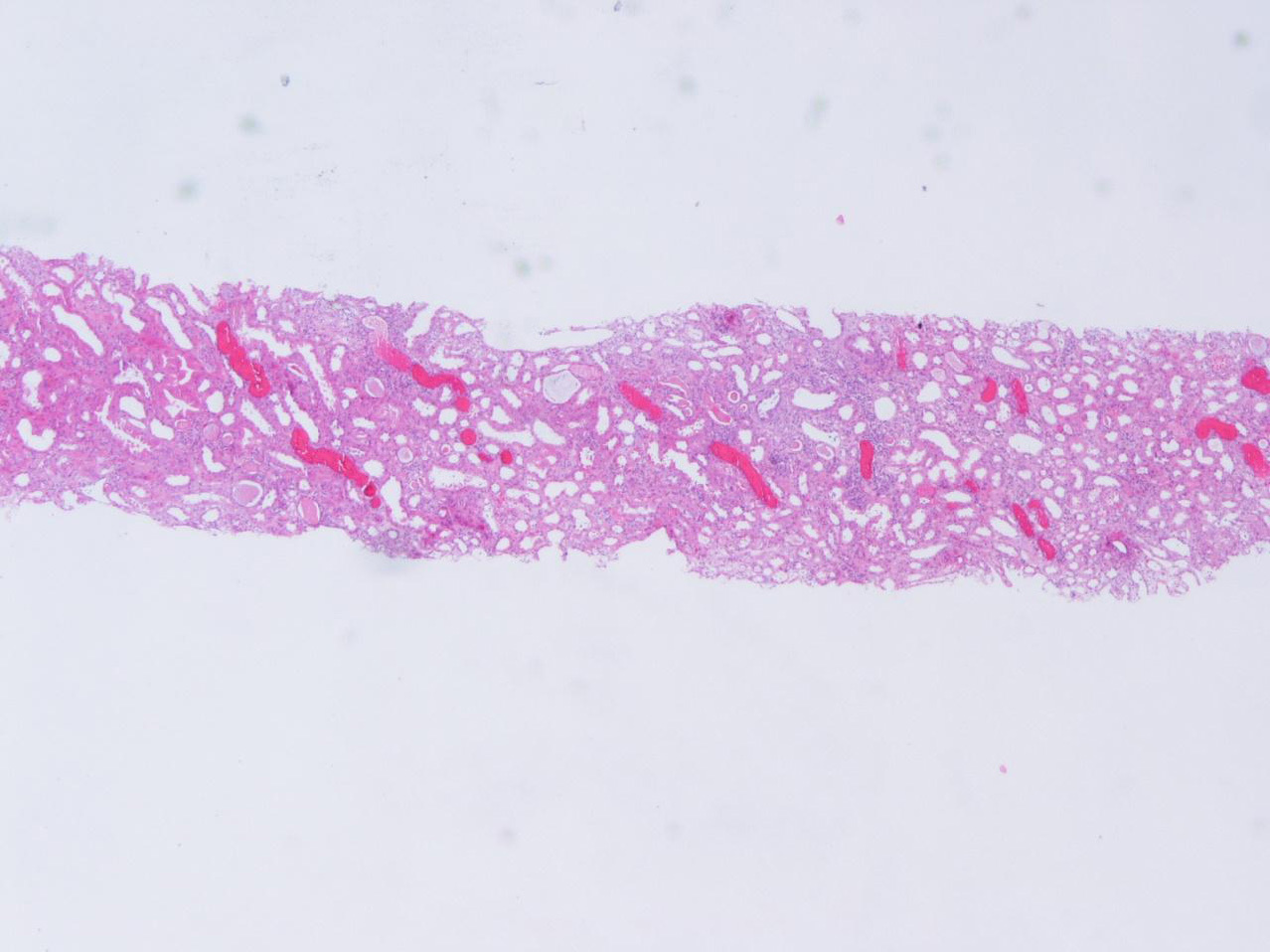
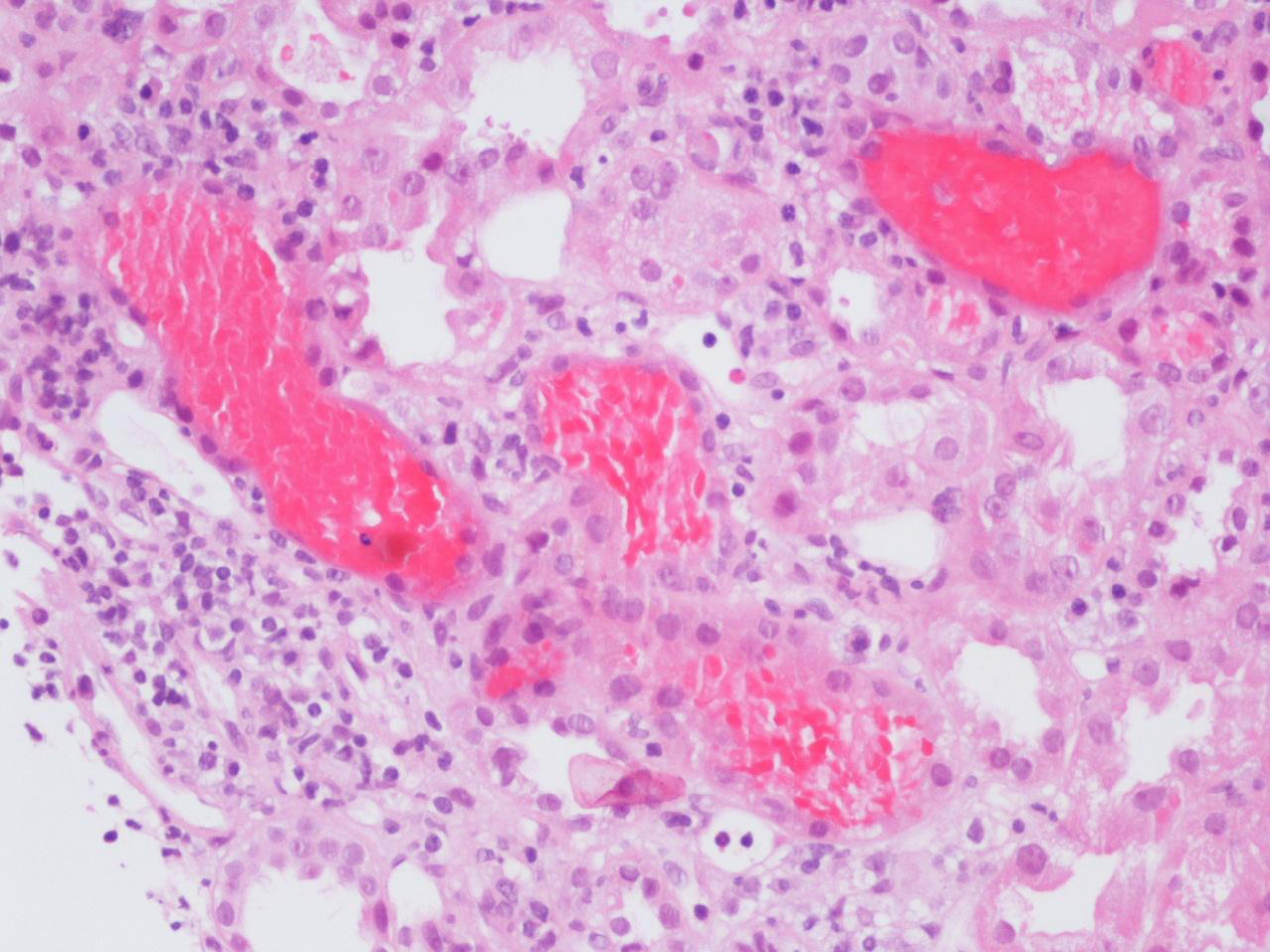
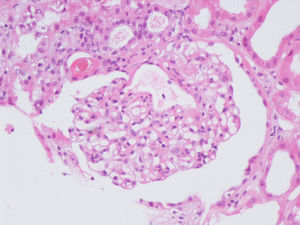
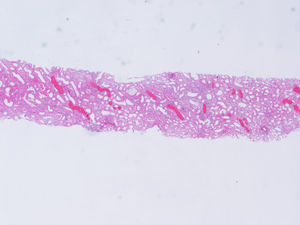
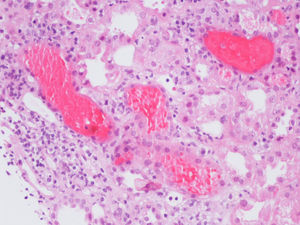
On the 14th day of hospitalization he had an episode of macroscopic hematuria. Blood pressure was 121/71mmHg and his physical examination was unremarkable. At that time hemoglobin was 10.7g/dL, creatinine was 3.5mg/dL and INR was 4.62. He became oliguric and was started on hemodialysis. A repeated renal ultrasound showed no obstruction. Serum complement levels were normal and no monoclonal immunoglobulins were detected. Serology for hepatitis B virus, hepatitis C virus and human immunodeficiency virus was negative. Anti-neutrophil cytoplasmic antibody and anti-glomerular basement membrane antibody were negative. Light microscopy of a needle renal biopsy containing 25 glomeruli showed diffuse mesangial proliferation. RBCs were found within the tubular lumina with formation of occlusive RBC casts in 10% of tubules. The occlusive RBC casts were mostly localized in distal nephron segments. On immunofluorescence (IF) staining, predominant C3 deposits (1+) and IgG (1+) were noted in the mesangium and capillary loops (Figure 1, Figure 2 and Figure 3). No glomeruli were available for electronic microscopy analysis. The patient did not recover renal function and remained on chronic dialysis.
Discussion
Warfarin therapy is associated with several adverse effects on kidney. In recent years, episodes of macroscopic hematuria and AKI in patients under treatment with warfarin have been increasingly described and have raised considerable interest.2,3,4 This entity has been called warfarin-related nephropathy (WRN) and the leading mechanisms are being explored. Initially, it was thought that WRN was only secondary to tubular obstruction by RBC casts, resulting in backflux of glomerular filtrate and increased renal cortical interstitial fluid pressure compressing adjacent tubules. However, several studies have been developed and have suggested the involvement of hemoglobin nephrotoxicity in its pathogenesis.
This entity was first reported by Abt et al that observed glomerular hematuria in a patient with excessive warfarin anticoagulation and underlying structural abnormality of glomerular basement membrane (GBM).5 Kabir et al reported a similar syndrome in a patient with inactive systemic lupus erythematous and abnormally thick GBM.6 This finding was also noted by Brodsky et al who reviewed renal biopsy findings from nine patients on warfarin therapy with unexplained AKI associated with increased INR, after excluding acute or active glomerulonephritis.2 All these patients had underlying kidney disease. The biopsy specimens revealed RBCs in both Bowman spaces and tubules. Clinical outcome in these patients was unfavorable, with incomplete recovery in up to 66% of patients. This was consistent with a subsequent study, in which it was estimated that among CKD patients over-anticoagulated with warfarin the incidence of WRN was about 37%, and suggested that these patients experience a faster progression of CKD.7
In effect, there is increasing evidence for an association between WRN and adverse renal outcomes. Recently, Moreno et al published a great editorial review about the impact of glomerular hematuria in the progression of CKD, suggesting that more accurately monitoring of hematuria and specific interventions to decrease hematuria or protect from its adverse effects may improve renal function outcomes in hematuria-induced AKI or CKD.8
The risk of WRN seems to be particularly high in patients with underlying kidney disease but it was recently suggested that WRN may also occur in non-CKD patients. In a study developed by Brodsky et al, WRN occurred in 33% of CKD and 16% of non-CKD patients. WRN patients had a lower survival rate at 1 year than over-anticoagulated patients without AKI. Survival at 1 year was lower in CKD than in non-CKD patients with WRN, with an increased 1-year mortality risk of 65% among CKD-patients.3
Interestingly, WRN seems to do not require severe warfarin coagulopathy, since previous works did not find significantly higher INR levels in WRN than in no-WRN patients and it was not established a significant correlation between the degree of INR level and the magnitude of serum creatinine increase.7
Our patient had underlying kidney disease and he presented with AKI and macroscopic hematuria. Based on the renal biopsy findings, we suggest that this was caused by severe glomerular hematuria, as was demonstrated by the finding of numerous renal tubules filled with RBC and RBC casts, and lack of evidence of bleeding from other sites in the urinary tract. In our case, as in most cases described, clinical outcome was unfavorable as dialysis dependence is common.
Physicians involved in the clinical care of patients on systemic anticoagulation therapy should be aware of this serious complication of warfarin therapy and carefully monitor coagulation parameters and kidney function in these patients. Anticoagulants should be stopped, if possible, or decreased while macroscopic hematuria is present, as excessive warfarin anticoagulation seems to increase the likelihood of WRN.
Since gross hematuria might only develop in patients with underlying kidney disease, it has been suggested that gross hematuria, not uncommonly seen in patients receiving systemic anticoagulation, could be a sign of an undiagnosed subjacent glomerulopathy such as structurally abnormal GBM or an inflammatory glomerulopathy and should not be attributed solely to the hypocoagulation.
Figure 1. Glomerulus showing moderate mesangial proliferation and increased mesangial matrix (hematoxylin and eosin stain).
Figure 2. Intratubular red blood cell (RBC) casts (haematoxylin and eosin)
Figure 3. Renal tubules are distended by numerous erythrocytes. The adjacent epithelial cells appear flat (haematoxylin and eosin).