Arterial hypertension is a highly prevalent disease and its secondary causes must always be kept in mind because the treatment and prognosis differ between these and essential hypertension. Here we present the first reported case in Argentina of a 21-year-old patient with arterial hypertension and hypokalaemia due to a renin-secreting juxtaglomerular cell tumour, which was diagnosed after seven years of development.
La hipertensión arterial es una enfermedad de alta prevalencia y siempre deben tenerse en cuenta las causas secundarias que pueden originarla, debido a que el tratamiento y el pronóstico difieren entre estas y la hipertensión esencial. Presentamos el primer caso reportado en Argentina de una paciente de 21 años con hipertensión arterial e hipopotasemia, debido a un tumor de células yuxtaglomerulares productor de renina, el cual fue diagnosticado tras siete años de evolución.
INTRODUCTION
Reninoma is a tumour of the cells of the juxtaglomerular apparatus that produces excessive amounts of renin, resulting in a secondary form of hyperaldosteronism, manifesting clinically with hypertension (HT) and hypokalaemia1. This renal tumour is predominant in females, with a peak incidence between the second and third decade of life and, although uncommon, it is a treatable cause of HT2. It should be suspected in any patient with refractory HT associated with hypokalaemia and high levels of aldosterone.
We present the first case of reninoma reported in Argentina in a young woman with refractory HT and hypokalaemia.
CASE REPORT
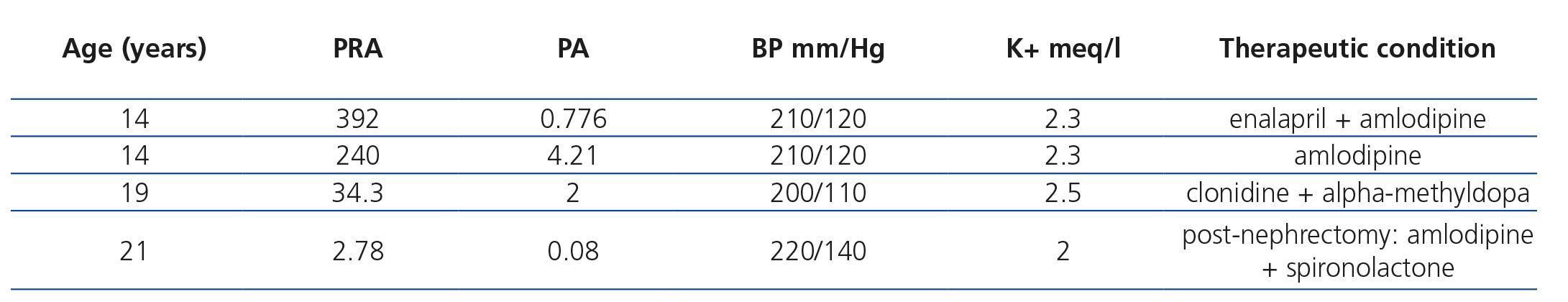
Female, diagnosed with HT at 14 years of age, when she was admitted for the first time to a paediatric hospital, with blood pressure (BP) of 210/120mmHg; headaches and hypokalaemia. When secondary HT was suspected, various studies were carried out. Renal ultrasound, echocardiography and catheterisation of the aorta and renal arteries did not display abnormalities. Plasma renin activity (PRA) and plasma aldosterone (PA) doses were high on two occasions (Table 1). Vanillylmandelic acid levels in urine and those of TSH, free T4 and T3 in plasma were normal. She was discharged from hospital on medication with angiotensin-converting-enzyme inhibitors and calcium channel blockers, but she did not return for follow-up tests.
At the age of 19, she consulted another hospital due to HT. She was eight weeks pregnant, and as such, she was hospitalised in intensive care. Good foetal health, BP of 200/110mmHg and hypokalaemia were determined, and she began treatment with clonidine and alpha-methyldopa. In the renal ultrasound in the lower pole of the left kidney there was a regular nodule formation 45mm in diameter, consistent with angiomyolipoma. PRA and PA levels were high. She continued outpatient treatment with labetalol and nifedipine. At 19 weeks of pregnancy, she was admitted through the emergency department, with the diagnosis of miscarriage and a curettage of the uterus was carried out. Four days later, she requested voluntary discharge, and did not return for follow-up tests.
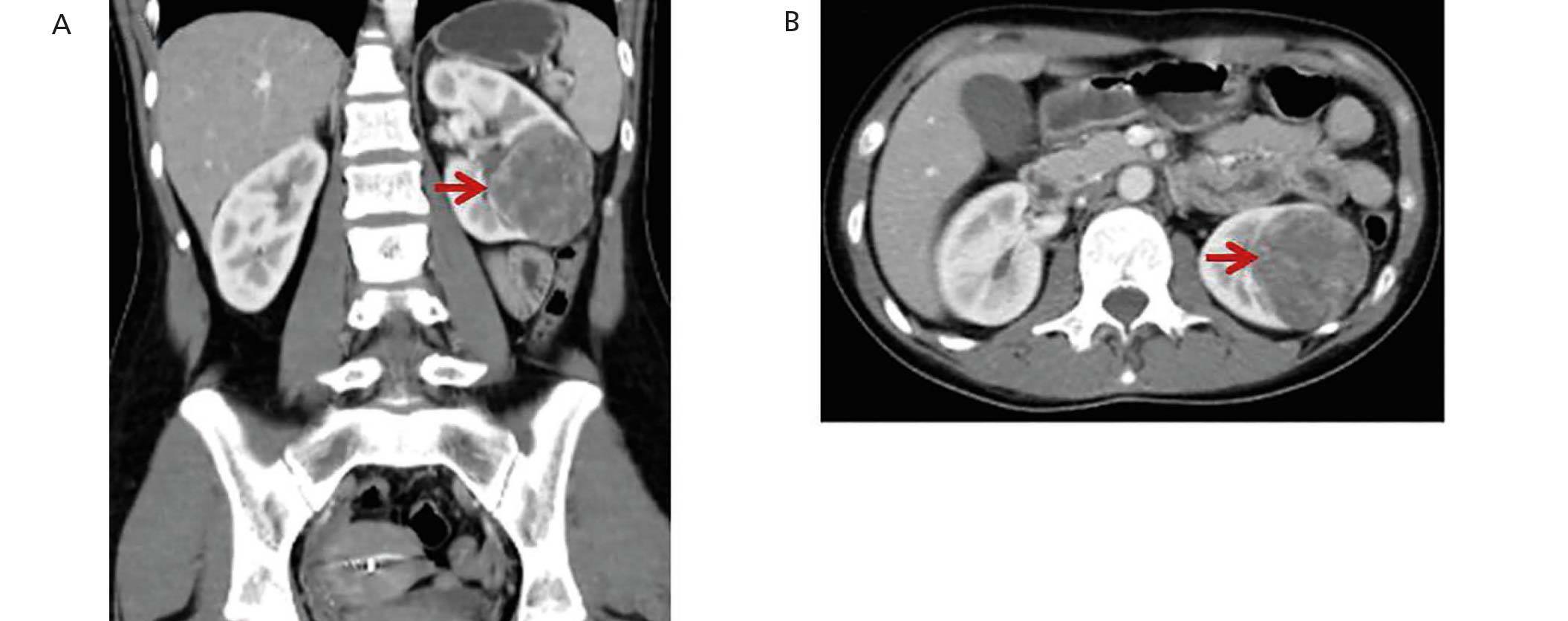
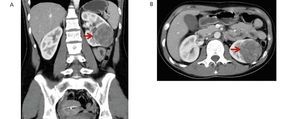
Two years later, on medication with enalapril, losartan and amlodipine, she was admitted to the emergency department of our hospital due to occipital neuralgia and muscle weakness lasting several days. She had BP of 220/140mmHg. In the initial studies, hypokalaemia of 2mEq/l, plasma creatinine of 0.6mg/dl and plasma urea of 25mg/dl were detected. The renal ultrasound displayed the image of a solid nodule, confirmed by abdominal computerised tomography with contrast, in which a solid, voluminous, hypervascular, space-occupying formation of 65mm in diameter was observed in the interpolar and lower pole sector of the left kidney (Figure 1). The ultrasound and Doppler ultrasound of renal arteries did not show abnormalities.
Given the presumptive diagnosis of HT secondary to renal tumour due to the high levels of renin and having ruled out other secondary causes of HT in previous studies, we decided to carry out a nephrectomy of the affected kidney. BP was controlled beforehand by adding spironolactone at doses of 100mg/day to her regular medication.
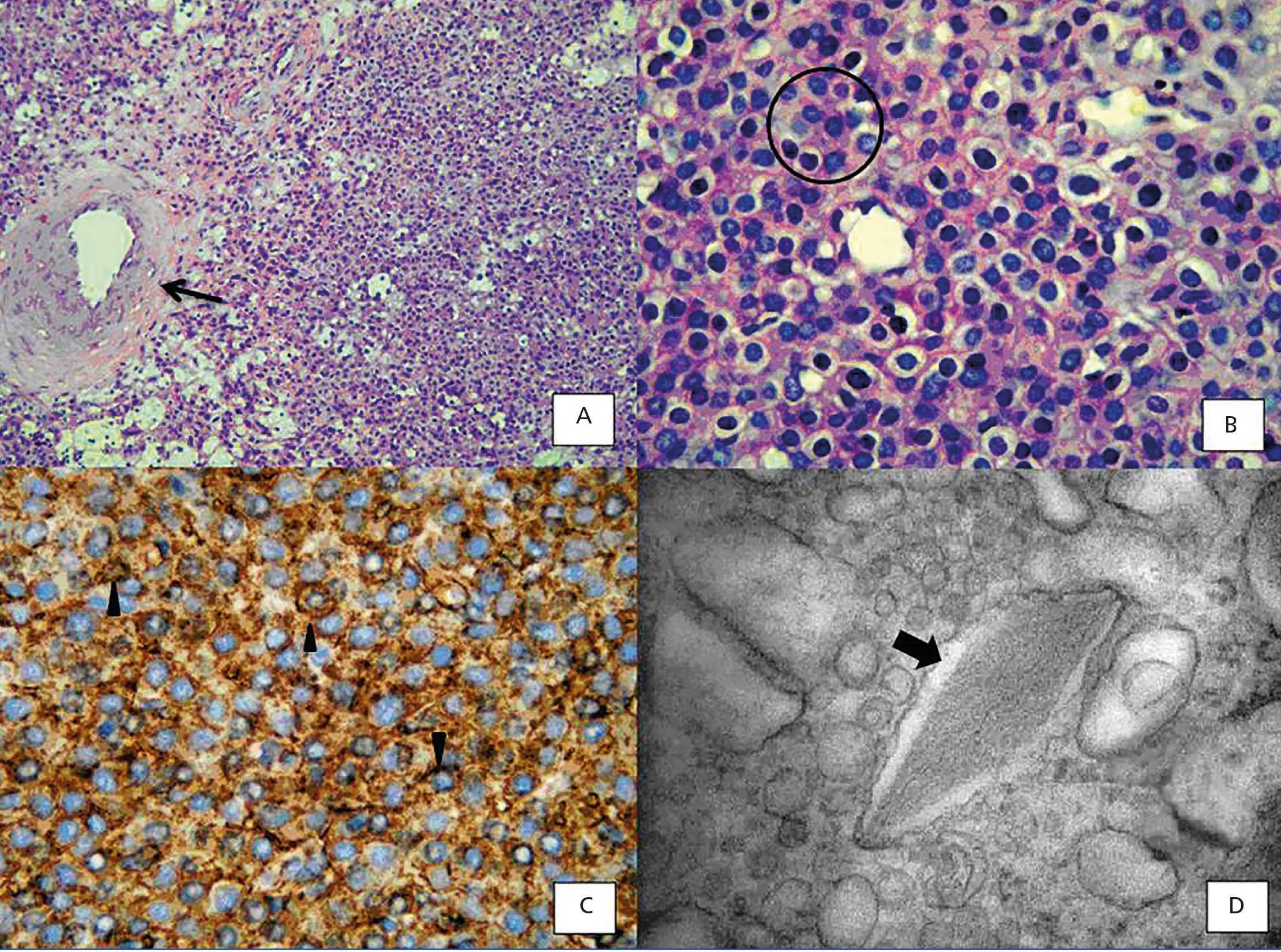
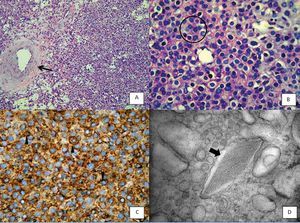
The pathological test revealed an encapsulated tumour of 5.5x4.5cm, with haemorrhagic appearance and whitish fibrous areas. Under the microscope, the tumour lesion consisted of medium-sized cells with medium, vesicular nuclei with irregular chromatin, some with inconspicuous nucleoli and eosinophilic cytoplasm, others with clear cytoplasm arranged in a diffuse pattern with extensive haemorrhage and mild mononuclear inflammatory infiltrate (Figures 2A and 2B), without invasion of the renal capsule. No cellular atypia, mitosis or necrosis were found. Tumour cells were positive for vimentin and showed strong and diffuse positivity for CD34 (Figure 2C). Observation at the ultrastructural level helped us to identify cells with intracytoplasmic granules with varying degrees of electro-lucidity, surrounded by membranes. With regard to the morphology, they varied from round to elongated, and there were some shapes with straight edges. In some of them, we also observed a crystalloid rhomboid shape which at high magnifications displays a zigzag structure with marked electron density (Figure 2D). These findings could be linked to a juxtaglomerular cell tumour (JCT), which allowed confirmation of the clinical suspicion.
After surgery the patient’s BP gradually decreased and the antihypertensive drugs were simultaneously withdrawn. The clinical course was asymptomatic and normotensive, with normal plasma renin, aldosterone and serum potassium, without drug treatment.
DISCUSSION
The association between HT and hypokalaemia generally indicates the diagnosis of hyperaldosteronism. High PRA and PA values allow the differential diagnosis between primary and secondary hyperaldosteronism3,4. If there is hyperreninemic hyperaldosteronism and HT, a differential diagnosis must be carried out between renal artery stenosis, coarctation of the aorta and a renin-secreting tumour5.
In 1967, Robertson et al.6 reported the first renin-producing tumour. Kihara et al. later called them “juxtaglomerular cell tumours”7. These tumours are very uncommon, with their incidence peaking between the second and third decade of life and they are predominantly found in females, originating in the myoendocrine cells of the renal juxtaglomerular apparatus, although the production of renin by different tumours has also been demonstrated, such as Wilms tumours, carcinoid tumours, renal oncocytoma and renal cell carcinoma8,9. In accordance with the presence or absence of symptoms, JCT may occur as: a “typical” variant in the majority of cases and manifests with HT, hypokalaemia, high plasma renin and secondary hyperaldosteronism; an “atypical” variant, in which HT is not accompanied by hypokalaemia; and a third “non-functioning” variant, which occurs without HT and with normal levels of potassium10,11.
JCT are located in the renal cortex and in the early years of their existence they may be undetectable using common imaging methods, and as such the selective measurement of renin in each renal vein may be required for its diagnosis12. Catheterisation of the renal arteries, as well as ruling out the presence of stenosis in the latter, may detect an avascular area corresponding to the tumour site. A dynamic CT scan shows a typical pattern that helps us to distinguish this tumour from others, manifesting as a hypovascular mass in the arterial phase, with moderate contrast uptake in the late phase. MRI is an option for very small tumours13.
The anatomapathological and immunohistochemical studies (immunoreactivity for markers: CD34, vimentin, CK7 and cytokeratin CAM5; variable staining for CD117 and smooth muscle actin, and negative for von Willebrand factor, CD31, desmin, S-100 protein, melanosome-associated antigen, chromogranin A, synaptophysin and neuron-specific enolase), together with the transmission electron microscope, which revealed the presence of cells with protogranules and mature renin granules, allowed us to confirm the clinical suspicion and perform the differential diagnosis with other tumours, such as renal cell carcinoma, haemangiopericytoma and metanephric adenoma14. While JCT are considered to be benign tumours, there may be vascular invasion, such as in the case reported by Shera et al., who demonstrated vascular invasion of the tumour capsule and a lymph node, with the disease recurring after one year15.
There have been few studies on its molecular genetics. Trisomy of chromosome 10, monosomy of chromosomes 9 and X, and the loss of most of the arm of chromosome 11q are the most commonly detected disorders16.
The removal of the tumour through surgery consistent with the size normalises levels of potassium, renin and aldosterone, and in most cases it also normalises BP levels17.
Normally, these tumours are diagnosed 5-7 years after the onset of HT, and as such, when there is HT and hypokalaemia, the PRA and PA should be studied. If both have increased and the patient is being treated with diuretics, coarctation of aorta and renal artery stenosis should be ruled out by Doppler ultrasound, CT-angiogram or arterial catheterisation.
In conclusion, JCT is a very uncommon cause of secondary HT and about 100 cases have been reported in the literature since 1967. This is the first case reported in our country and it was diagnosed after several years of evolution, since the tumour was not initially observed despite numerous tests, which could suggest that the clinical manifestations begin with microscopic lesions. In these cases, the selective dosage of renin in each renal vein would be a useful tool for diagnosing the kidney affected.
Acknowledgements
We would like to thank Dr Eduardo Bravo, Dr Ricardo Pedernera and Dr Vanesa Perrone for their cooperation in the patient follow-up during hospitalisation. Lastly, we are grateful for Ms. Elena Pereyra’s technical assistance with the transmission electron microscope.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Values for plasma renin activity, aldosterone, blood pressure and potassium levels
Figure 1. CT images of the left renal tumour (arrows)
Figure 2.
12623_16025_61630_en_12623_19115_61630_es_12623_tabla1_en.doc
Table 1. Valores de actividad de renina plasmática, aldosterona, presión arterial y niveles de potasio