Antecedentes: La biopsia percutánea de injertos renales es un método diagnóstico para la evaluación, manejo y seguimiento clínico del trasplante renal, por lo cual es necesario conocer sus complicaciones. Existen pocos datos en la literatura en relación con las complicaciones derivadas de las biopsias en injertos renales. Objetivo: Evaluar la tasa de complicaciones de las biopsias realizadas en injertos renales en nuestro centro. Pacientes y métodos: Estudio observacional retrospectivo. Se incluyeron las biopsias de injertos renales realizadas entre enero de 2000 y septiembre de 2012. Se definieron como complicaciones mayores: anemización que requirió transfusión sanguínea, fístula arteriovenosa intraparenquimatosa o sangrado arterial que requirieron embolización, trasplantectomía, otro tipo de cirugía y exitus. Y como complicaciones menores: anemización sin transfusión sanguínea, fístula arteriovenosa intraparenquimatosa sin embolización, hematomas o colecciones perirrenales, hematuria y fiebre. Las biopsias renales fueron realizadas bajo control ecográfico y con dispositivos automáticos. Resultados: Se realizaron 390 biopsias a injertos renales. Se produjeron 49 complicaciones. Veintidós fueron mayores: 12 por anemización que precisaron transfusión sanguínea, 6 requirieron embolización (5 por fístulas arteriovenosas y 1 por sangrado arterial), 2 exitus, 1 trasplantectomía y 1 intervención quirúrgica (por hematoma). Veintisiete fueron menores: 12 colecciones perirrenales, 9 fístulas arteriovenosas sin embolización, 3 hematurias, 2 anemizaciones sin transfusión sanguínea y 1 fiebre. Conclusión: La tasa de complicaciones relacionadas con la biopsia del injerto renal observada en nuestro centro es similar a las descritas sobre riñones nativos; por lo tanto, consideramos que es también una técnica segura y eficaz, y una importante herramienta diagnóstica.
Background: Percutaneous biopsy of renal grafts is a diagnostic method for the assessment, management and clinical monitoring of renal transplant, so it is necessary to know its complications. There are few data in the literature regarding complications from biopsies in renal grafts. Objective: To evaluate the rate of complications in renal graft biopsies performed at our centre. Patients and Method: We performed a retrospective observational study, including data from patients who underwent renal graft biopsies from January 2000 to September 2012. Major complications were defined as: anemia requiring blood transfusion, intraparenchymal arteriovenous fistula or arterial bleeding requiring embolisation, nephrectomy, other surgery and exitus. And as minor complications: anemia without blood transfusion, intraparenchymal arteriovenous fistula without embolisation, haematomas or perirenal collections, hematuria and fever. Kidney biopsies were performed with ultrasound guidance and automatic devices. Results: We performed 390 kidney graft biopsies. 49 complications occurred. 22 were major: 12 per anemia that required blood transfusion, 6 requiring embolisation (5 arteriovenous fistulae and 1 arterial bleeding), 2 exitus, 1 trasplantectomy and 1 surgery (haematoma). 27 were minor: 12 perirenal collections, 9 arteriovenous fistulae without embolisation, 3 hematuria, 2 anemisation without blood transfusion and 1 fever. Conclusions: The rate of complications related to renal graft biopsy observed in our centre is similar to those described for native kidneys, therefore we believe it remains a safe and effective technique, and an important diagnostic tool.
INTRODUCTION
Renal biopsy is a procedure that has contributed to the knowledge of kidney disease since 1950. In the case of kidney grafts, it is a recognised diagnostic method for their evaluation, management and clinical follow-up. It is also of great value in determining graft prognosis and viability.1 In Spain more than 70% of the indications for renal transplant biopsies are due to diagnosis reasons.2
This is an invasive technique and although in most cases there are no complications, there is always some risk,3 so it is individually indicated after assessing the risk/benefit ratio for each patient.4
Its main contraindication is the presence of a coagulation disorder. All other contraindications are relative, such as hypertension and suspected infection.4
The most common complications are prolonged gross haematuria (5-10% of cases), perirenal haematoma and intrarenal arteriovenous fistula. Almost all patients have microscopic haematuria and up to 12% have gross haematuria that is usually self-limiting and disappears with rest in a few hours. If it affects the collecting system, it can lead to urethral obstruction. If there is haemorrhage into the retroperitoneal space, there can be complications such as decreased haemoglobin and hypovolaemia. If there is active bleeding, endovascular procedures such as selective embolisation of the bleeding vessel may be necessary. About 1% of cases required transfusion and 0.1% required embolisation. Surgery was necessary to control bleeding in 0.1% to 0.4% of cases, nephrectomy in 0.3%, mortality rate is below 0.1%.5,6
Renal biopsy should ensure that sufficient and representative material from the renal cortex is obtained for an adequate diagnosis while minimizing possible complications associated with the process. In this regard, the use of real-time ultrasound to guide the process and the use of automatic biopsy needles has improved success rates up to 95%, thus reducing the incidence of complications.7 However, there is discussion regarding the use of different calibre puncture needles.2 At present, there are three sizes of needles for renal biopsies: 14, 16 and 18G. Naturally, higher gauge needles (14G) make it possible to obtain more tissue, but their use is often associated with increased discomfort to the patient8 and to an increased incidence and extent of post-biopsy haematomas and a significant reduction in haematocrit values.9 Indeed, the use of such needles is now infrequent and 16-gauge needles are preferred as they provide a better chance of obtaining a suitable amount of tissue with fewer complications. In general it is advisable to always obtain two cylinders to ensure adequate sample size.
Our objective was to determine the rate of major and minor complications of renal graft biopsies performed during the period from January 2000 to September 2012 in the Nephrology Department of the La Paz General University Hospital.
PATIENTS AND METHOD
A retrospective observational study was conducted over a period of 13 years, in which 390 renal graft biopsies, performed between 1 January 2000 and 30 September 2012 in the Nephrology Department of La Paz University Hospital were included.
All biopsies performed were ultrasound-guided (transducer Sector, MultiHertz, Sonoline G20, Siemens) with automatic needles (16 or 18-gauge automated cutting ACECUT ®, TSK needles). No surgery or biopsy was performed by the transvascular route.
Prior to the procedure, all patients underwent blood and coagulation tests, 7 day washouts of oral anticoagulants and antiplatelet agents, and suspension of heparin 24 hours before.
After the procedure no routine renal ultrasounds were performed, unless complications were suspected. In the case of programmed procedures, patients were admitted for a minimum 24 hour hospital stay.
Renal biopsy complications were divided into major and minor according to degree of medical intervention and/or surgery. Major complications were defined as: anaemisation requiring blood transfusion, intraparenchymal arteriovenous fistula with embolisation, arterial or venous bleeding requiring embolisation, transplants or other surgery and deaths.
Minor complications were defined as: anaemisation not requiring blood transfusion, intraparenchymal arteriovenous fistula not requiring embolisation, perirenal haematomas or collections, haematuria and fever.
The following variables were analysed: age, sex, aetiology of chronic renal failure, months from kidney transplant to renal biopsy, number of biopsies performed on the renal graft, presence and type of complications associated with renal graft biopsy, pathology diagnoses, date and cause of graft loss, and date and cause of death.
RESULTS
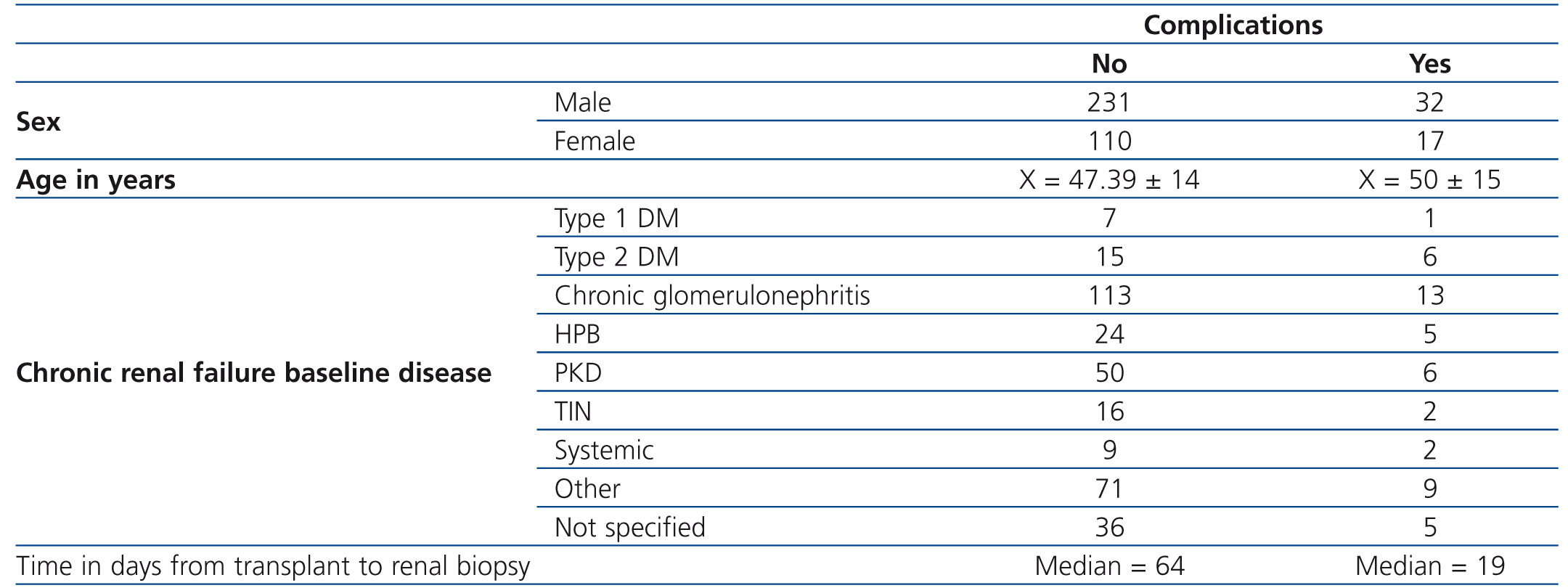
We analysed 390 biopsies in 256 patients with renal transplants from January 2000 until September 2012, with a mean of 30 biopsies/year. In Table 1 are detailed demographic characteristics of the patients, as well as the time between graft and biopsy in renal transplant patients, depending on the presence or absence of complications related to renal biopsy.
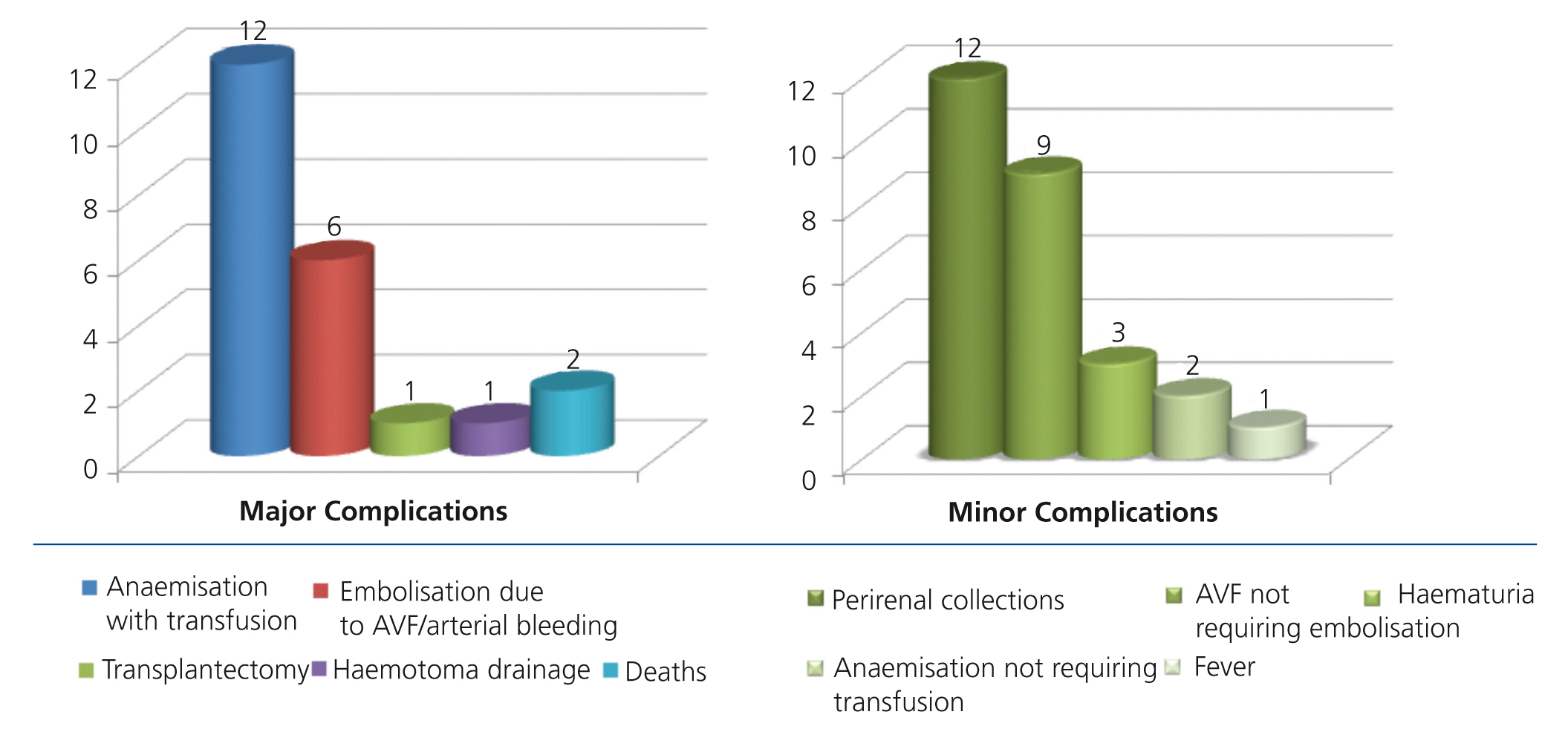
The total number of complications observed in kidney graft biopsies was 49, which corresponds to an overall rate of 12.6%, of which 22 were major complications (5.6%) and 27 were minor complications (6.9%).
Of the 22 biopsies with major complications, there were 12 cases of anaemisation which required blood transfusions (3.1%), 6 embolisations, one of them due to intrarenal arterial bleeding and 5 (1.5%) due to intrarenal fistulae, 1 nephrectomy secondary to bleeding due to post-biopsy major laceration of the lower pole kidney graft (0.3 %), 1 required surgery for evacuation of perigraft haematoma secondary to renal biopsy (0.3 %), and finally there were 2 deaths (0.5%), both women, of 58 and 71 years of age, who had arterial bleeding secondary to renal graft biopsy, requiring embolisation and who suffered hypovolemic shock which required admission to the intensive care unit (ICU). In the case of the 71-year-old patient, while in the ICU she suffered septic shock secondary to hospital-acquired pneumonia and multiple organ failure and died 21 days after her renal graft biopsy. The other patient died after 26 days in the ICU with infections of respiratory and urinary origin.
Of the 27 biopsies with minor complications, 12 were perinephric collections (3.1%), 9 arteriovenous fistulae not requiring embolisation (2.3%), 3 haematuria (0.8%), 2 anaemisations not requiring blood transfusion (0.5%) and one episode of fever (0.3%) (Figure 1).
The number of biopsies of a single renal graft ranged from 1 to 5, with a mean of 1.5. The most frequent was a single biopsy (65.6%) and the least frequent was 5 biopsies of a single renal graft (1%). The success rate in obtaining tissue for histopathology was 97.9%.
DISCUSSION
In our experience, renal graft biopsies are a safe and effective technique for obtaining samples of renal parenchyma in transplant patients. Over a period of 13 years in our hospital our overall complication rate was 12.6%, major complications 5.6% and minor complications 6.9%. These results are similar to those seen in other studies of renal biopsies of native kidneys, with a complication rate of 8% to 16%, with a greater percentage of minor complications, similar to those seen in our study.10,11 However, there is little data on complication rates of renal graft biopsies. In the literature reviewed we only found a 1994 German study, in which the complications of 458 kidney biopsies both of native kidneys and renal grafts comparing different biopsy techniques, both manual and automatic, are described. Of all the biopsies performed, 143 were of renal grafts, 50 were performed using a manual technique and 93 an automatic needle technique, a complication rate of about 30% in renal grafts was seen irrespective of the technique used, and a similar percentage in native kidneys; the percentage in renal grafts using automatic needles was far greater than that found in our study.12
While it is true that the rate of major complications in our study was 5.6 %, which is higher than the rates observed in some Spanish series on complications associated with native kidney biopsies,13,14 there are other series with results similar to ours in which major complication rates of up 6.4% were recorded. The most serious complication, although not the most frequent, we saw in our sample, was the death of 2 patients (0.5%). We believe that, as this is a very low percentage, renal graft biopsy remains a safe procedure, although this mortality rate is higher than that reported in other studies.5,6
The most common minor complication observed in our study were perirenal collections, followed by arteriovenous fistulae that did not require embolisation, haematuria, anaemisation not requiring transfusion and fever.
Of the 390 biopsies performed, the success rate in obtaining tissue for histopathology was 97.9%, which is similar to that reported in other studies.10-12
No relationship was found between the number of biopsies performed on the same renal graft and the occurrence of complications; indeed, in the grafts that underwent 3 to 5 biopsies, the complication rate was minimal and these were mostly minor complications.
In our centre, tissue was obtained using 16 G x 150 mm and 18 G x 200 mm needles. We do not have sufficient data to relate needle calibre to complication rate, while other studies have found that changing from an 18G to a 16G needle did not increase morbidity but did increase diagnostic results.13
In conclusion, based on data obtained, we can say that renal graft biopsy is as safe and effective as native kidney biopsy and provides valuable information for accurate diagnosis and treatment decisions. We consider it advisable to perform it when required, given that the benefit will be greater than the risk to which the patient is subjected, due to the low rate of complications observed.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Demographical characteristics, aetiology of chronic renal failure and time elapsed from transplant to renal biopsy in relation to the presence or absence of complications
Figure 1. Major and minor complications of biopsies of renal grafts.