Increase in aldosterone level is a known cause of secondary hypertension which can be suspected relatively ease in clinical practice, especially if it is accompanied by hypokalaemia, and if it constitutes severe or sudden-onset hypertension.1 However, certain diagnostic difficulties may arise when specifying its origin, particularly in cases with increased levels of both renin and aldosterone2,3 and in which imaging tests do not help to establish an aetiological diagnosis.
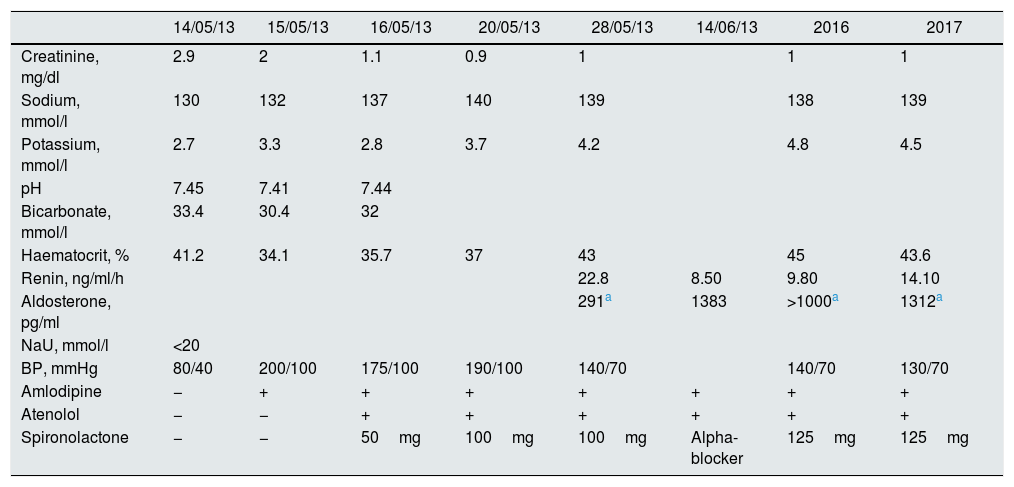
A 62-year-old female with a personal history of hypertension (untreated), dyslipidaemia and obesity, who smoked one packet of cigarettes/day. The patient went to her health centre complaining of urinary incontinence along with polyuria and polydipsia which had been ongoing for one month. Measurement of blood pressure (BP) was 220/130mmHg. The patients was stated on captopril 50mg/12h along and atenolol 50mg was prescribed, and she was scheduled to the outpatient nephrology clinic the following day. When she attended the nephrology clinic (having taken 50mg of captopril that morning), she was found to be experiencing bradypsychia, she was slow to react, with a BP of 80/40mmHg, requiring 0.9% physiological saline solution. The computed tomography (CT) scan of the brain was normal. The lab test values from the first consultation and the following days in Table 1. In 2011, serum creatinine was 0.9mg/dl, and imparement of kidney function was attributed to the treatment of hypertension with captopril, with renal recovery in the following days. Given the presence of hypertensive crises, with a tendency to hypokalaemia, along with urinary sodium of less than 20 mmol/l, lead to the suspicion of hyperaldosteronism. Given the history of hypotension following captopril, in a smoker with dyslipidaemia, it was suspected hyperaldosteronism secondary to artery stenosis. A renal Doppler ultrasound was requested (right kidney measuring 13.2cm and left kidney measuring 11.2cm, with normal renal blood flow), as well as an angio-CT which showed calcified atheroma adjacent to the origin of the right renal artery, without significant stenosis, and a permeable left renal artery. The suprarenal glands were also normal on the abdominal CT scan, therefore primary hyperparathyroidism could be ruled out. After the effect of captopril disappeared and following fluid replacement, her BP increased and it was necessary to gradually introduce amlodipine and atenolol. In light of suspected hyperaldosteronism, spironolactone was introduced. The first renin and aldosterone test (performed under treatment with 50mg of spironolactone) showed elevated levels renin with aldosterone levels within the normal range. Given the increasing suspicion of hyperaldosteronism, this test was repeated, suspending therapy with spironolactone beforehand, confirming aldosterone levels of above 1000pg/ml, with elevated renin activity. Hyperaldosteronism was therefore confirmed, although the imaging tests were not conclusive to classify it as primary or secondary. Over the following years, aldosterone was blocked with spironolactone, and acceptable BP control was also achieved with amlodipine and atenolol, with persistently elevated renin and aldosterone levels. On her most recent control abdominal CT scan, a nodular image measuring 1.7cm, suggestive of adenoma, was observed in the right suprarenal gland, which was not present four years earlier.
Analytical progression, blood pressure and treatments used.
| 14/05/13 | 15/05/13 | 16/05/13 | 20/05/13 | 28/05/13 | 14/06/13 | 2016 | 2017 | |
|---|---|---|---|---|---|---|---|---|
| Creatinine, mg/dl | 2.9 | 2 | 1.1 | 0.9 | 1 | 1 | 1 | |
| Sodium, mmol/l | 130 | 132 | 137 | 140 | 139 | 138 | 139 | |
| Potassium, mmol/l | 2.7 | 3.3 | 2.8 | 3.7 | 4.2 | 4.8 | 4.5 | |
| pH | 7.45 | 7.41 | 7.44 | |||||
| Bicarbonate, mmol/l | 33.4 | 30.4 | 32 | |||||
| Haematocrit, % | 41.2 | 34.1 | 35.7 | 37 | 43 | 45 | 43.6 | |
| Renin, ng/ml/h | 22.8 | 8.50 | 9.80 | 14.10 | ||||
| Aldosterone, pg/ml | 291a | 1383 | >1000a | 1312a | ||||
| NaU, mmol/l | <20 | |||||||
| BP, mmHg | 80/40 | 200/100 | 175/100 | 190/100 | 140/70 | 140/70 | 130/70 | |
| Amlodipine | − | + | + | + | + | + | + | + |
| Atenolol | − | − | + | + | + | + | + | + |
| Spironolactone | − | − | 50mg | 100mg | 100mg | Alpha-blocker | 125mg | 125mg |
BP: blood pressure; NaU: urinary sodium.
Reviewing the literature, Zorzi et al. describe a case of a 41-year-old male who had been studied 14 years earlier due to suspected secondary hypertension (including renin and aldosterone, with this screening being negative). Years later, he was re-assessed due to worsening of his BP values. A unilateral aldosterone-producing adenoma was found in this re-assessment, which had not previously been detected in the initial screening, with the authors concluding the need to perform clinical follow-up.4 In our case, the initial clinical data (severe hypertension along with hypokalaemia and a urinary sodium value of <20mmol/l, and severe hypotension following captopril) also pointed to hyperaldosteronism, which was confirmed analytically, although the initial imaging tests did not help to establish the cause of excess aldosterone. We therefore believe that these patients with excess aldosterone, in whom a specific cause cannot be found, should be blocked with anti-aldosterone agents and. In addition, patients should undergo strict follow-up, not only for BP control, but also periodic re-assessments of imaging tests, which could help to reveal a hidden aetiology of hyperaldosteronism.
Please cite this article as: Benito MH, Fernández-Reyes Luis MJ, Rodríguez Gómez MA. Aldosteronismo con actividad de renina aumentada: ¿primario versus secundario? Importancia del seguimiento en el tiempo para el diagnóstico. Nefrologia. 2019;39:102–103.